For many patients grappling with severe bruxism, the world of dental restorations has been a conundrum with limited options. The standard choices—including zirconia, porcelain-fused-to-metal (PFM), and full-cast crowns—are effective but often bring their own limitations. But a transformative solution has been making waves in dentistry, one that mimics the brilliance of modern vehicle design, where crumple zones and safety features shield passengers from harm during an accident. Enter the era of 3D printed final restorations: a boon for patients, particularly those with a habit of grinding and gnashing.
Gordon Christensen, DDS, PhD, MSD, of Clinician’s Report has aptly likened zirconia crowns to the vehicles of the 1960s and 1970s, robust and formidable on the outside but lacking the critical ability to absorb and distribute forces effectively. Zirconia, as we have come to know, can be unyielding, literally a piece of metal that can wreak havoc on opposing dentition. The analogy becomes more evident when you imagine fusing this unyielding material with a titanium implant, creating a setup that lacks the flexibility to cushion the blows of occlusal forces. Such rigidity can significantly increase the risk of implant failure and exacerbate wear on the opposing teeth.1-3
Now, fast-forward to the 21st century, where dentistry is experiencing its own evolution. The equivalent of crumple zones and protective features in modern vehicle design can be found in 3D printed final restoration crowns. These remarkable creations possess the capacity to mimic the natural wear of tooth enamel, combining strength with a built-in fail-safe mechanism.
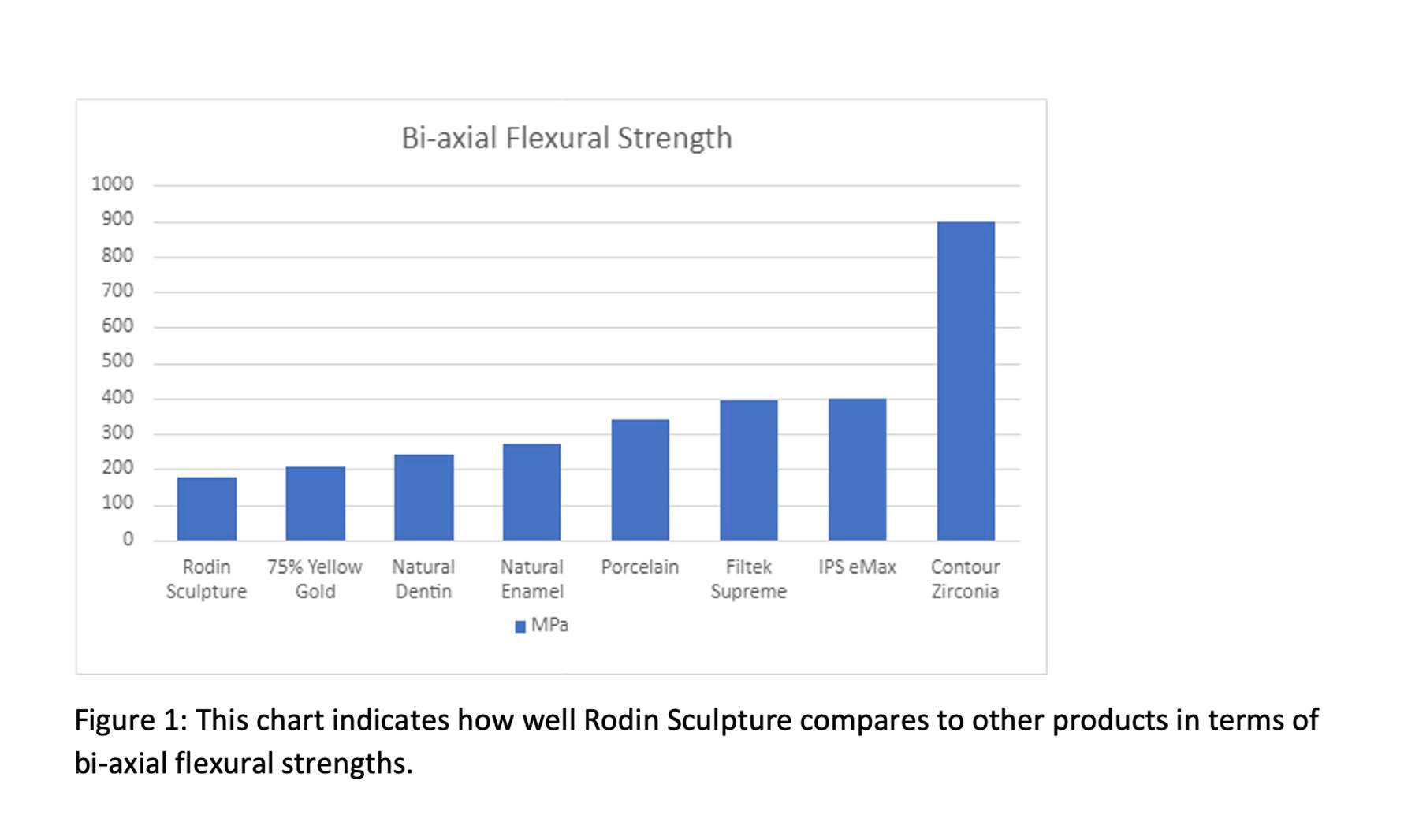
Pac-Dent’s Rodin Sculpture, a ceramic-filled nanohybrid 3D printable resin, measures an impressive 175 MPa, presenting a dental material closely approximating the natural properties of dentin (240 MPa) and enamel (270 MPa). When compared with more traditional alternatives such as PFM (340 MPa), 3M’s Filtek Supreme (395 MPa), Ivoclar’s IPS e.max (400 MPa), and contour zirconia (900+ MPa), it emerges as a standout choice, especially when compared with the cost of precious and nonprecious full cast options (Figure 1).5-7
This 3D printed resin is not only strong but also exhibits the potential to mimic the wear and function of natural tooth structure. Its superior biomechanical compatibility, with properties that align more closely with natural dentition, makes it an optimal selection for dental restorations. The ability to endure the rigors of occlusal forces while providing a more natural feel and wear pattern positions printed resin as a remarkable advancement in dental material science, promising resilience and a restoration that closely replicates the function of the patient’s original dentition.8
Printed resin also offers a unique property of breaking when necessary to protect the implant, the abutment, and, most importantly, the surrounding bone from the destructive forces of bruxism. The journey into the realm of 3D printed crowns has ushered in an era of resilience and cost-effectiveness. This is especially significant for individuals with a proclivity for grinding their teeth, a habit that can test the durability of any dental restoration. Heavy bruxers and grinders are known to exert formidable forces that can challenge even the most robust materials. In some extreme cases, perfectly placed implants and abutments have been snapped in half by the relentless lateral forces generated by bruxism. In such situations, 3D printed crowns become an invaluable alternative to traditional options like zirconia and PFM.9-11
Figure 1. This chart indicates how well Rodin Sculpture compares to other products in terms of bi-axial flexural strengths.
Figure 2. This kit from Pac-Dent offers unparalleled control and precision, enabling users to achieve optimal esthetic results. Available in a diverse range of shades, clinicians can easily customize restorations, ensuring a perfect blend with patients’ dentition and resulting in a seamless, great-looking smile.
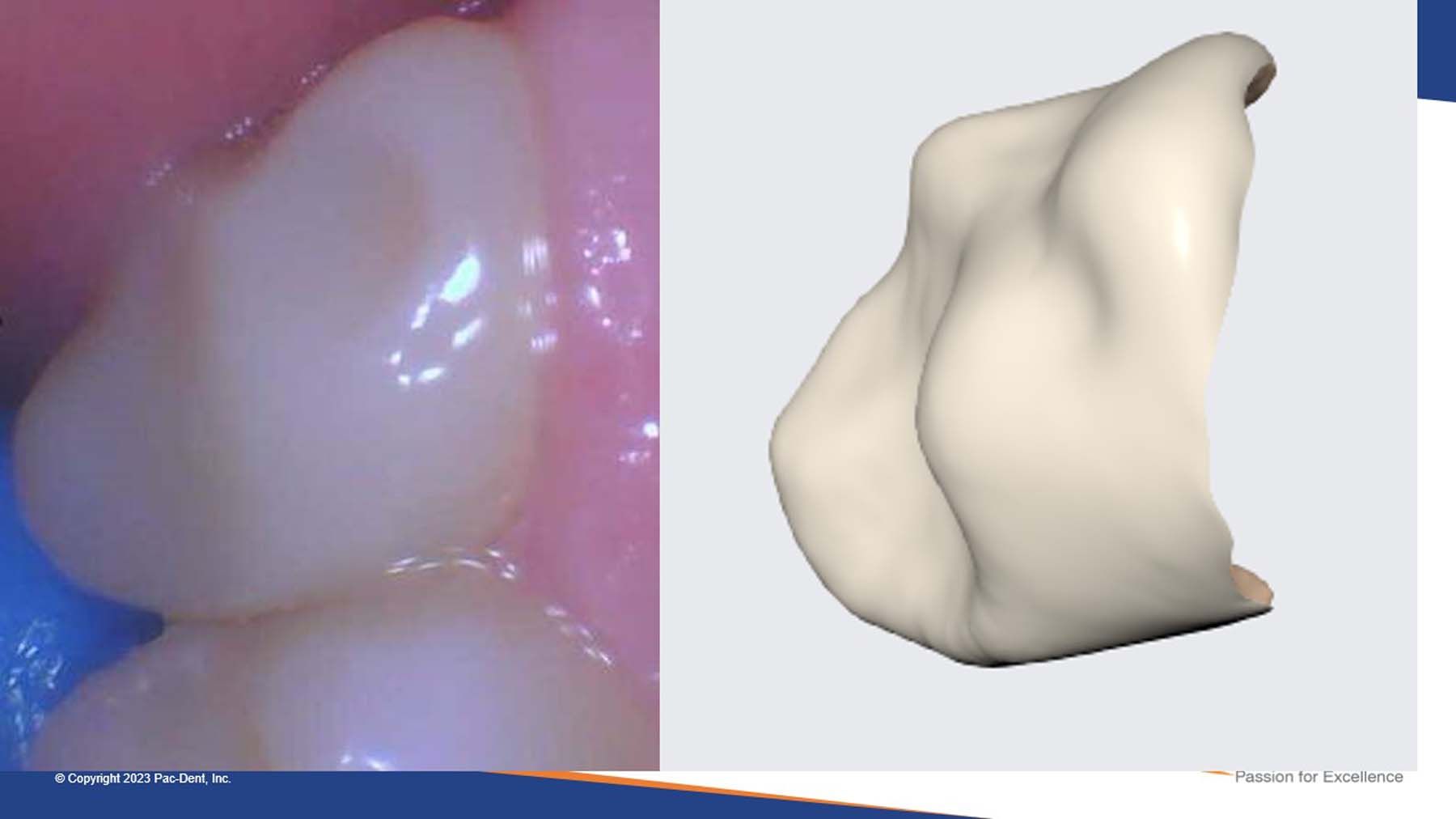
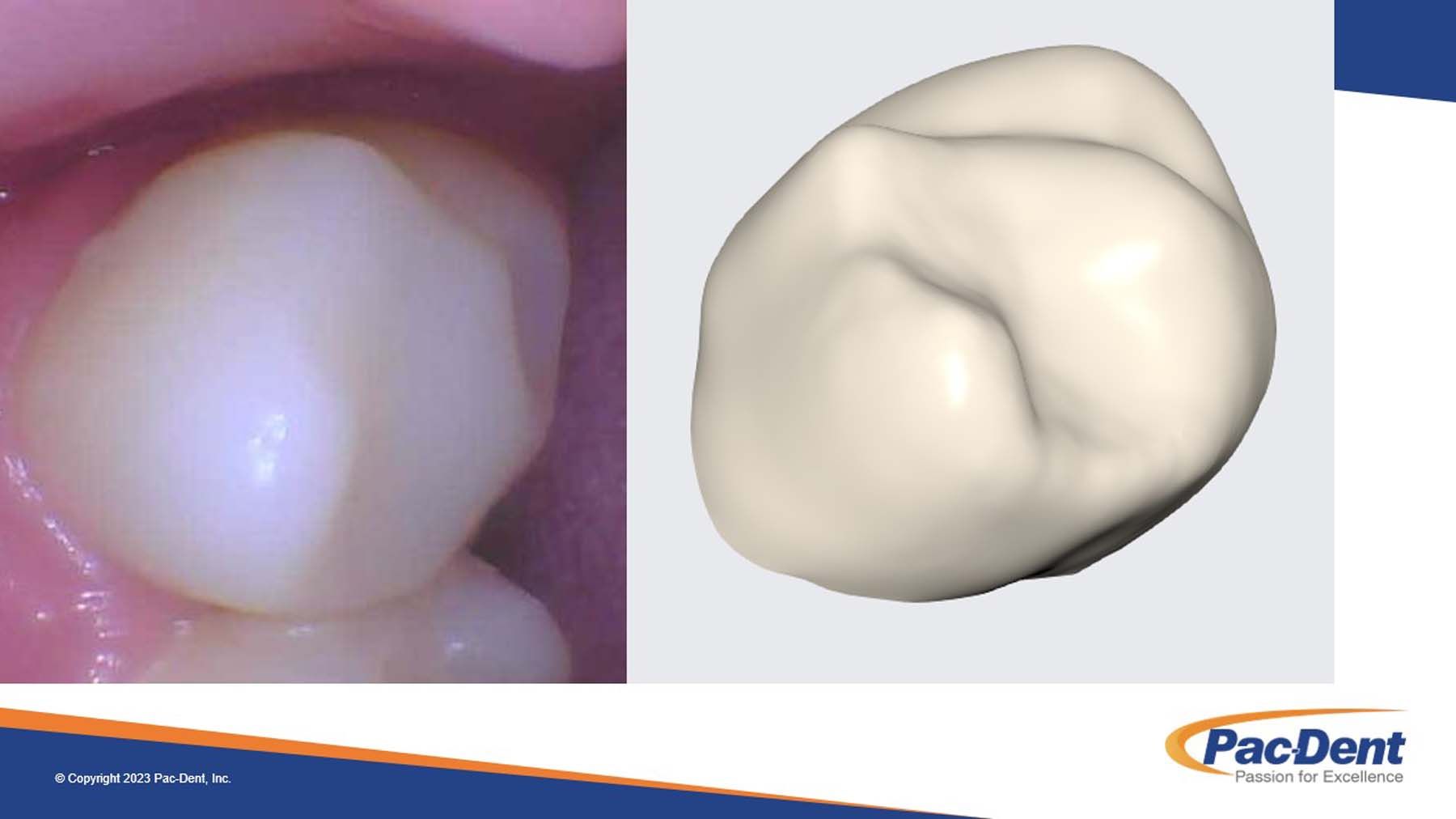
Figures 3a and 3b. Durable and resilient: the restorations showed no color or shade changes months later, and the surrounding tissues remained healthy.
Figures 3a and 3b. Durable and resilient: the restorations showed no color or shade changes months later, and the surrounding tissues remained healthy.
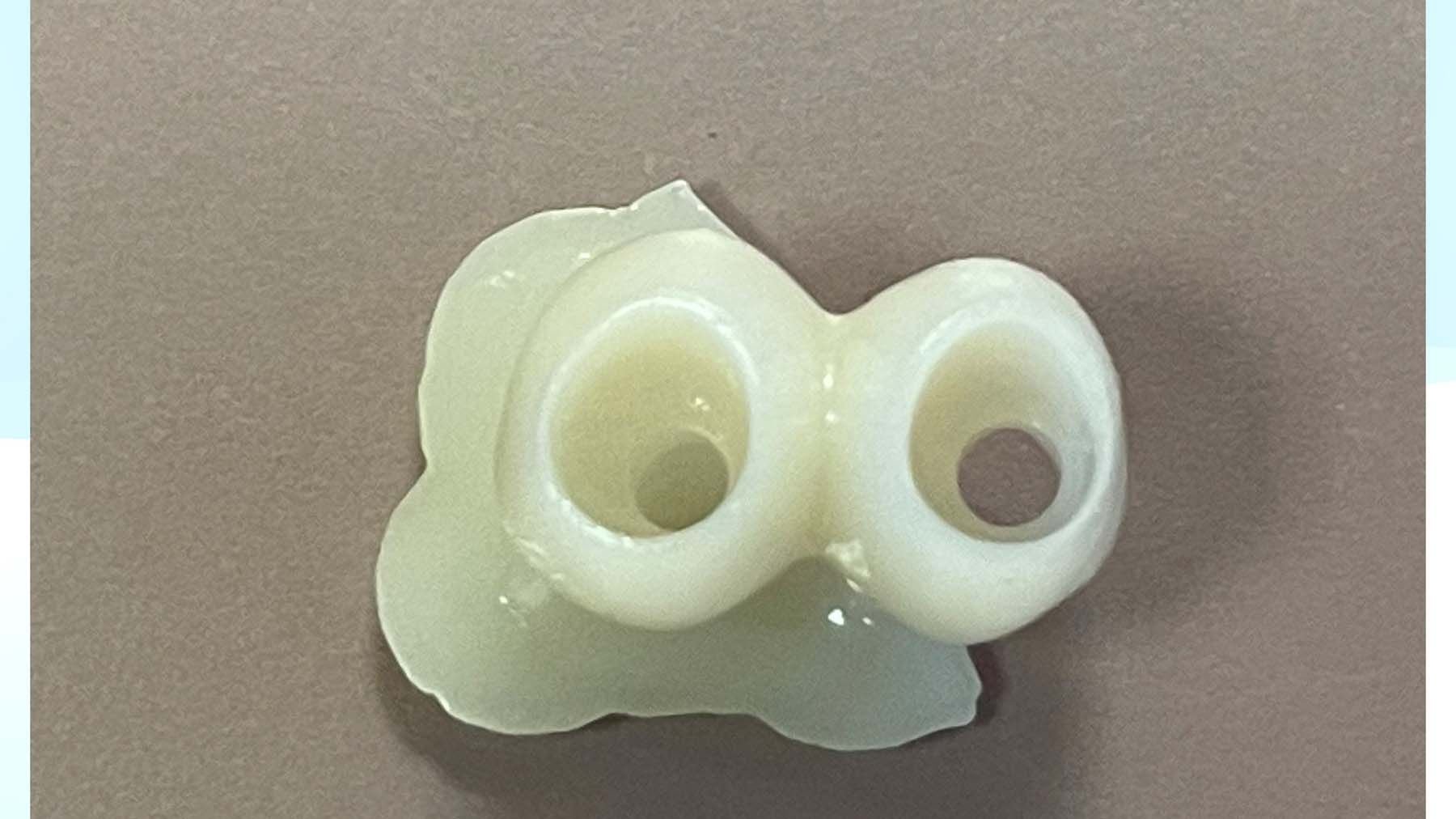
Figure 4. Bottom view of the marginal edge of printed crown.
Figure 5. Buccal view of the printed crowns with support.
Figure 6. Buccal view of the printed crowns without support.
One important point to consider concerns insurance reimbursements for printed crowns. Although these crowns are technically resin-based, it is noteworthy that Pac-Dent played a pivotal role in advocating for their inclusion in the American Dental Association materials group approved as of 2023. Printed resins with filler content exceeding 50% are now recognized as ceramic restorations eligible for reimbursement, like PFM and zirconia.
What sets these printed crowns apart is their ability to be quickly and easily duplicated, ensuring patients can access cost-effective replacements with minimal hassle. This not only saves patients time and money but also averts the need for expensive subsequent surgeries in case of failure. Moreover, the balanced properties of these crowns have the potential to reduce wear and tear on opposing dentition, a critical consideration for long-term oral health.12,13
Case Study: Comprehensive 3D Printed Restorations for Implants #4 and #5
Patient Information:
Name: John Doe Age: 54 years
Gender: Male Dental history: Good oral hygiene, recent extraction of teeth #4 and #5 due to severe decay and infection
Presenting Complaint:
John Doe presented to our dental clinic with a chief complaint of missing teeth #4 and #5, which recently had been extracted due to severe decay and associated infections. He was eager to explore the best options for replacing these teeth and was particularly interested in innovative, efficient, and cost-effective solutions.
Clinical Evaluation:
Upon clinical examination and discussion with the patient, it was determined that the best course of action was to proceed with dental implants to restore the functionality and esthetics of his smile. I had successfully placed dental implants in the #4 and #5 positions. After 4 months, the implants had fully integrated with the bone, exhibiting excellent stability of 78 on the Osstell ISQ Scale and readiness for the next phase of treatment, which involved the fabrication of custom restorations.
3D Digital Impressions:
In preparation for 3D printed restorations, digital impressions with implant scan bodies were taken using our state-of-the-art intraoral scanner, the Medit i700. This technology allowed us to create precise digital models of the implant sites and the surrounding dentition. The accuracy of these digital impressions is paramount for the success of the 3D printed restorations, ensuring a snug fit and natural occlusion.
Design and Planning:
The digital impressions were exported to exocad to meticulously plan the restorations. Each crown and custom abutment were designed to provide optimal occlusion, esthetics, margins, and comfort. The 3D design process allowed for the fine-tuning of every detail, ensuring that John’s new teeth would seamlessly integrate into his smile. I have initiated training for my assistant in crown design, and she has enthusiastically embraced this new responsibility. With exocad’s intuitive artificial intelligence crown design generation, she has even managed to create designs in under 5 minutes.
3D Printing Process:
Once the designs were finalized, the crowns were uploaded to Ackuretta’s slicing software, ALPHA AI. Printing supports were automatically generated, and the design was ideally automatically positioned on the build plate of the Ackuretta SOL printer. The crowns were printed within an hour. We had a choice of utilizing either the Rodin Sculpture 2.0 or the Rodin Titan resins from Pac-Dent. The main difference was that the Titan has a flexural modulus strength much lower than Sculpture. Because this was only a 2-unit bridge and not much longer, without requiring the additional flexibility and high-impact strength, Sculpture 2.0 was selected. As for the custom abutments, those were milled by my local lab technician.
The restorations emerged with remarkable precision. These 3D printed crowns displayed the ideal combination of strength, esthetics, and durability, making them an excellent choice for implant restorations. The total estimated in-house cost, including the milled abutments, crown resin, and design labor, came to roughly $180.
Figure 7. The healing abutment implant site #4 and #5
Figure 8. A view of the gingival emergence profile of the implant site #4 and #5.
Figure 9. The custom abutments in place.
Figure 10. The printed crown is seated with no try-in and no cement.
Figures 11 and 12. Figure 11 shows the printed crown seating with cement and the implant screw, while Figure 12 is a look at the final cementation and the implant screw.
Figures 11 and 12. Figure 11 shows the printed crown seating with cement and the implant screw, while Figure 12 is a look at the final cementation and the implant screw.
Post Cure:
Postcure procedures include the following crucial steps in the final preparation of the crowns: first, thorough cleaning with light brushing. The crowns are rinsed in 99% alcohol to remove any residual resin and contaminants, ensuring a clean and biocompatible surface. The printing supports are removed and all surfaces are trimmed and finished with a fine slow-speed acrylic carbide. Following this cleaning process, crowns undergo UV curing, which can be achieved using specialized equipment like the Otoflash G171 curing unit. This unit emits a controlled dosage of UV light to further enhance the crown’s full mechanical strength properties and biocompatibility, making it a critical step in the production of 3D printed restorations.
Restoration Placement:
With the 3D printed restorations prepared, John returned to our clinic for the final phase. I conducted a meticulous assessment of the crowns, focusing on their fit and esthetics while ensuring light occlusion with anatomical contacts. Fortunately, no adjustments were necessary. The next step involved cementing the restorations with Rodin luting cement and bonding them to the abutments using Rodin Bond. To achieve the desired esthetic outcome, I employed the versatile Rodin Palette Naturalizing Kit, enhancing the restoration through a skillful application of stain and glaze (Figure 2).
This process elevated the overall shade, hue, and chroma to achieve optimal esthetics. The staining and glazing materials, designed specifically for 3D printed resins and resin based, allowed for convenient touch-ups during the seating process.
Outcome:
The result was a resounding success. John Doe’s new 3D printed crowns for teeth #4 and #5 fit flawlessly into his smile. Not only did they restore the functionality of his missing teeth, but the esthetics were so natural that they seamlessly blended with his existing dentition. He left our clinic delighted with his rejuvenated smile.
Nearly 4 months later, it is incredibly encouraging to note that John’s crowns continue to exhibit remarkable durability and resilience. The restorations showed no color or shade changes, and the surrounding tissues remained healthy. The biocompatibility of zirconia-filled resins appears comparable to that of contour zirconia.
In a compelling testament to the enduring quality of Rodin Sculpture’s 3D printed crowns, I had the privilege of connecting with Aaron Welch, DDS, another early 3D final resin adopter. Dr Welch provided documented evidence of printed crowns he had placed over 2 years ago, displaying minimal signs of wear and demonstrating their exceptional longevity in bruxism studies (Figure 3a-3b). This extended durability underscores the enduring excellence that this advanced approach to dental restorations offers to patients like John.
With 3D printed restorations, we have opened the door to a new era of affordable dental prosthetics, where precision, customization, and patient satisfaction take center stage.
References
1. Koutsoukis, T, Zinelis, S. 3D Printing and Ceramics in Dentistry: A Review of Current and Emerging Applications. Dentistry Journal, 2021;9(4), 41.
2. Popov, I, Stavropoulos, A, Vandeweghe, S. Comparative in-vitro Evaluation of the Mechanical Properties of 3D-Printed PMMA and milled Denture Bases. BMC Oral Health, 2020;20(1), 175.
3. Ahrberg, D, Lutz, R, Furniss, D, Rueger, C. 3D Printing in Dentistry: State of the Art. Journal of Clinical Medicine, 2018;7(9), 179.
4. Salmi, M, Tuomi, J, Paloheimo, KS. Fused deposition modeling of novel scaffold architectures for tissue engineering applications. Journal of Cranio-Maxillofacial Surgery, 2013:41(1), 47-50.
5. Willems, G, Lambrechts, P,Bream, M, Vanherle, G. pubmed.ncbi.nlm.nih.gov/8272502/. National Library of Medicine –HIH – PubMed, (1993 Sep 1994).
6. 3M ESPE Filtek – 3M Center Building 275-2SE-3 St. Paul MN 55144-100 (2018). multimedia.3m.com/mws/media/629066O/filtektm-supreme-ultra-universal-restorative.pdf
7. CAD/CAM message board > Prosthodonitcs > Fixed Prosthodontics; Full Zirconia Vs. e.max Single Units. Dentaltown Message Board, dentaltown.com/images/dentaltown/magimages/0812/dtaug12pg46.pdf. Accessed Nov. 16, 2023.
8. Sun, Q, Sauvage, MC, Balani, K, Deng, X. Additive Manufacturing of Bioceramics for Bone Tissue Engineering. Comparison to Traditional Dental Materials, 2017;10(8), 898.
9. Wang, Y, Huang, W, Yang, Y, Zhao, Y. Comparative Study of Mechanical Properties and Microstructures of 3D Printed Zirconia and CoCr Dental Restorations. Comparison to Traditional Dental Materials,2020;13(9), 2182.
10. Corbani K, Hardan L, Skienhe H, et al. Effect of material thickness on the fracture resistance and failure pattern of 3D-printed composite crowns. Int J Comput Dent. 2020;23:225-233. PMID:32789310
11. Gad MM, Alalawi H, Akhtar S, et al. Strength and wear behavior of three-dimensional printed and prefabricated denture teeth: an in vitro comparative analysis. Eur J Dent. 2023 Jan 20. doi: 10.1055/s-0042-1759885. Epub ahead of print. PMID: 36669653.
12. Mangano, FG, Hauschild, U, Veronesi, G, Imburgia, M, Mangano, C. Trueness and Precision of Four Intraoral Scanners in Oral Implantology: A Comparative In-Vitro Study. PloS One, 2018;13(9), e0202916.
13. Savoye, J, Benington, PR, Al-Sabek, FW, et al. A Review of 3D Printing in Dentistry. British Dental Journal, 2019;226(10), 761-769.










 Download Issue: Dental Products Report February 2024
Download Issue: Dental Products Report February 2024

