How to use prototyping for profitability through predictability
Prototyping offers dental labs accuracy and reduced postdelivery failures.
Over the past decade, our industry has witnessed a definite advancement in technology-driven prosthetic solutions. Initially, many of these computer-aided design technologies were classified as “nice to haves,” but because technicians had no predictable way to bring the digital design into an analog world, the validity of many technologies was questioned.
Fortunately for the dental industry, the past few years spawned multiple new and very innovative materials to support these digital processes. This merging of materials and digital design has definitively answered the question: “Should I go digital?”
Prototyping offers the modern-day dental laboratory the ability to accurately transfer a digitally produced diagnostic wax-up to the patient’s mouth for evaluation and approval. This transitional step, along with the ability to process the final prosthesis in a full digital workflow, has greatly reduced the delivery stresses and, more importantly, postdelivery failures.
Currently, 2 technologies are available to transfer the digital design: additive and subtractive. The older, and therefore also the more established technology, is a milling solution. This technology had a head start on additive solutions, so the materials available for these milling units are more advanced. Unfortunately, reducing any material creates friction and friction leads to wear, which ultimately speeds up failure. A reductive technology is not only slower than an additive solution but also requires more maintenance and inherently has a slower production rate. Ultimately, most dental laboratories would rather produce products with printing technology because of its accuracy and scalability. At the time this article was written, our industry lacked esthetic printing materials appropriate for long-term intraoral use.
A prototyping workflow allows the patient a test-drive of the virtual final prosthesis and in return, gives a clinician the ability to make final adjustments. These fine-tune adjustments, while sometimes frustrating, were traditionally done at the final delivery.
Adjusting on a polymer or resin material versus a sintered zirconia structure is not only better for the longevity of the final material but also positively influences patient confidence and the clinician’s profitability.
Prototyping Options
Jack Marrano and his Advanced Restorative Team at Absolute Dental Services in North Carolina offer a prototype try-in appointment as a part of all complex cases. This “trial” device is part of Absolute’s suggested clinical workflow and is supplied with every complex case.
This device serves as a final bite check, model verification, and final esthetic try-in. Currently, Absolute offers 2 options—a disposable printed, and a dual-use milled prototype.
Disposable Printed Prototype
A printed, disposable prototype (Figure 1) is included with the regular workflow and offered to the clinician at no additional charge. The advantage of a printed try-in is that intraoral adjustments (either by adding composite or reducing with a bur) are easily done to the prototype itself. These adjustments allow for immediate feedback from the patient. The main disadvantage is that this printed try-in is a functional representation of the final and that esthetic results are not represented by this device. Furthermore, depending on the type of printed resin used, the prototype device can be worn by the patient for a short to medium term.
Formlabs Denture Teeth Resin (Figure 2; formlabs.com) is a biocompatible photopolymer resin that works great for this application. This material is categorized as a class 2 biocompatible resin and supports printing resolutions to 50 microns. The material displays flexural resistance capabilities of greater than 50 MPa and a density of 1.15 g/cm3 < X < 1.25 g/cm3.1
It is important to note that a printed structure’s material properties will greatly vary depending on several factors, including type of printer, print orientation settings, and temperature. Therefore, it is difficult to accurately determine and control mechanical properties like water sorption and solubility. These properties can greatly influence the longevity of a prosthesis as it relates to discoloration and material breakdown.
Dual-Use Milled Prototype
A dual-use prototype (Figure 3) is considered an Absolute Signature product and serves as a try-in and a long-term emergency hybrid. This transitional prototype gives a patient the ability to try-in an exact copy of what the final prosthetic proposal will be. This device is delivered to the patient with the final prosthesis and can be used as a long-term emergency hybrid.
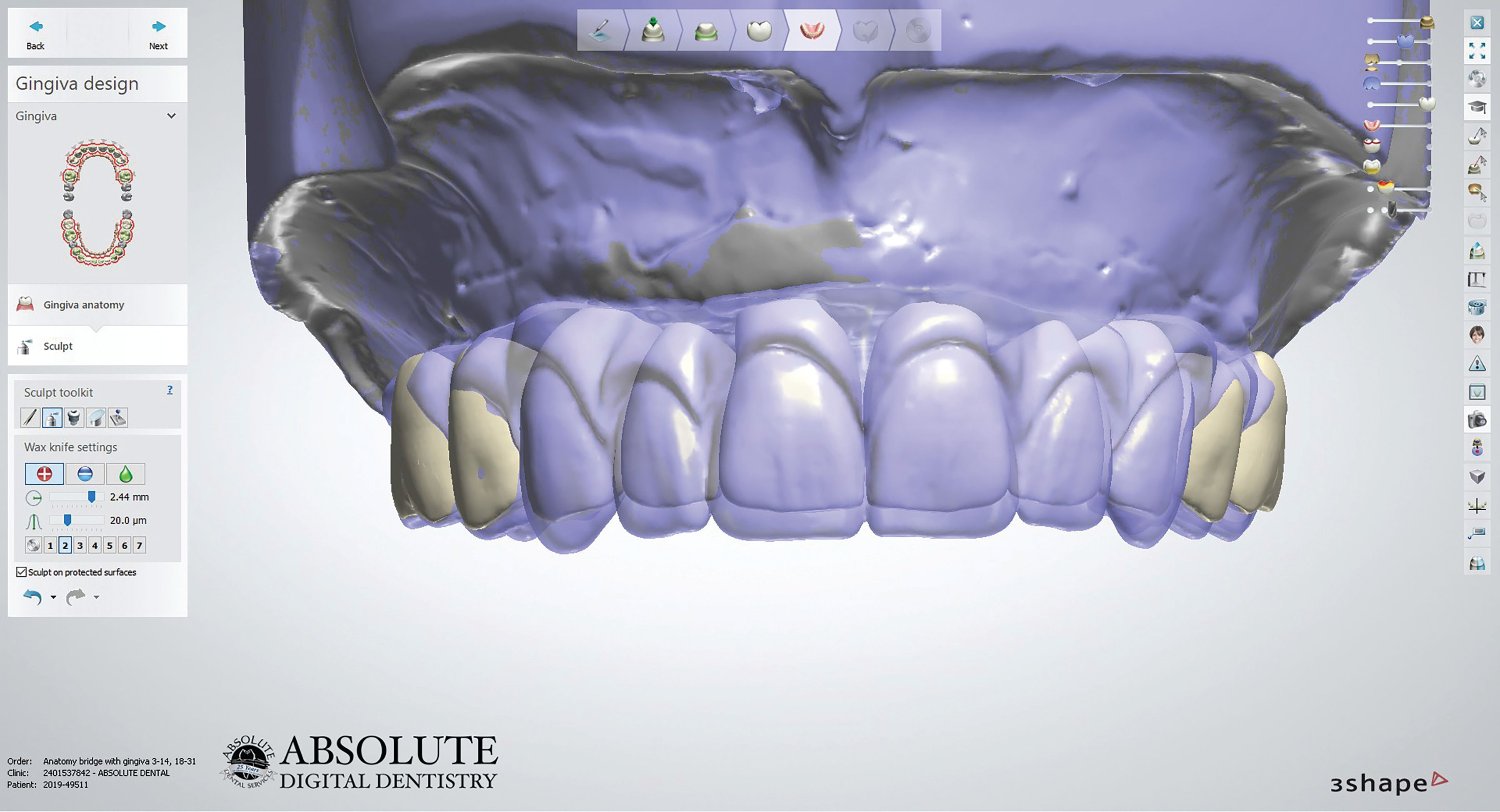
The advantage of working in this fully digital workflow when restoring a dual-arch rehabilitation is that the approved prototype will be fully interchangeable with the final prosthesis (Figure 4). This device, being an exact functional and esthetic copy of the final, gives the restorative team the ability to achieve a guaranteed patient approval before proceeding to the final restoration. Absolute Dental Services utilizes 3Shape design software (3shape.com) for the diagnostic, prototype, and final design (Figure 5). This software allows maintenance of all the progressive files—from preop to final—in one digitally interchangeable folder.
These prototypes are milled from double cross-linked polymethyl methacrylate–type materials (Figure 6). Absolute uses Harvest Dental’s Temp Esthetic. This double cross-linked polymer material is supplied in 98.5 and 95 mm millable pucks and is available in 12 popular Vita and bleach shades. The material is a multilayer composite allowing for very esthetic, long-term provisional results.
Temp Esthetic is Food and Drug Administration (FDA) 510(k) cleared for medium- to long-term use as a provisional material. Per data filed with the FDA, the device can remain in place for up to 5 years. Temp Esthetic displayed a flexural strength of greater than 100 MPa and water sorption under ISO 10477 of less than 20 µg/mm3, making this an exceptionally resilient intraoral material.2
Summary
Digital processes are key to efficiency and profitability. The question as to whether laboratories should process in digital has been answered. Material development is the next frontier.
References
1. Materials data sheet. Formlabs. September 18, 2018. Accessed November 5, 2020. https://archive-media.formlabs.com/upload/XL-DataSheet.pdf
2. Harvest Temp Esthetic. Package insert. Harvest Dental Laboratory Products LLC. Accessed October 2020. https://static1.squarespace.com/static/579bb6cf725e25911c5e632d/t/5e5ef0a942e056080e830a63/1583280297769/FRM-IFU-09+Rev5+-+DFU+Temp_Esthetic3.pdf






 Download Issue: Dental Lab Products December 2020
Download Issue: Dental Lab Products December 2020

