Warming to a New Bulk Fill Composite
I was recently introduced to VisCalor bulk by VOCO. Previously, I was using TPH Spectra® from Dentsply Sirona as my universal composite and Ivoclar Vivadent’s Tetric EvoCeram® as a bulk fill restorative option. I was initially hesitant to make the switch due to my loyalty to these excellent products, but after a colleague’s recommendation, I decided to give VisCalor a try.
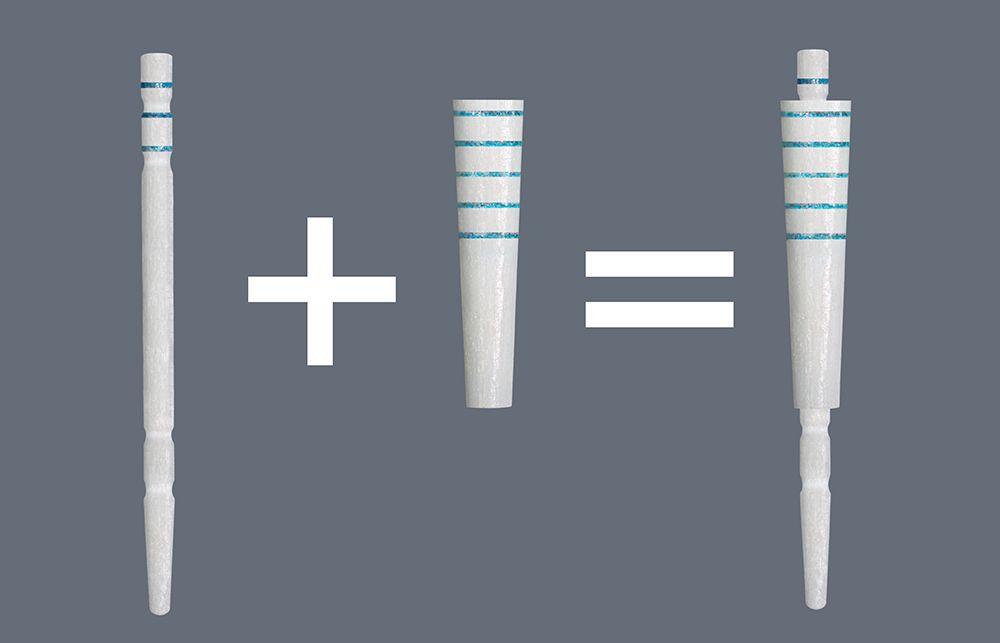
I’m glad I did! It has given us excellent results. Some features that make this product a great choice are the narrow cannulas and the marriage of the composite warmer and the thermoviscous technology. VisCalor bulk is easy to place, polishes well, and adapts extremely well in hard-to-reach preps. These attributes give the resin the ability to flow and adapt well, which is clearly evident on Class II restorations when you remove the sectional matrix. I am happy to say I have seen a significant improvement over my previous restorative protocols.
The VOCO composite warmer—provided as part of the system—has 3 temperature options. For a larger dental office with multiple dentists, the flexibility allows each provider to use it how they prefer. The previous composite warmer we used only had 1 setting, which made composites too hot and therefore not ideal for sculpting. The medium temperature setting seems to be the sweet spot to achieve ideal adaptation and shaping/carving parameters for good restorative dentistry.
Another key feature is having a universal shade that blends well for posterior esthetics. I was surprised how it still retained opacity to cover discolorations in teeth, which is a common issue with the bulk fill resins I have used in the past.
One thing to note about this product is that VisCalor bulk is intended and required to be used with the VOCO composite warmer or dispenser gun. It is a very difficult material to extrude when using the Cavifil version without heating the product.
Overall, VOCO’s VisCalor bulk has performed extremely well for us, and I am happy I switched to this for our bulk fill restorative needs. VOCO is a premium brand in the dental industry but seems to fly under the radar. With this product I believe they will do very well. Innovation is a key part of our practice, and we look forward to trying future VOCO products.

















 Download Issue: Dental Products Report September 2021
Download Issue: Dental Products Report September 2021

