Tip: Use CBCT to Educate Patients to Make Informed Treatment Decisions
From the most mundane decisions to the most important, we are used to having unlimited information at our fingertips to help decide whether we are making the right choice. So, when patients are told they need a crown or an extraction, they may balk. Ten years ago, there would have been no hesitation, but today Google, WebMD, and even Facebook are available for crowdsourcing information and opinions. It is more important than ever for doctors to use technology as a tool for educating patients about treatment while instilling confidence that the decision to proceed is right for them.
Show, Do Not Just Tell
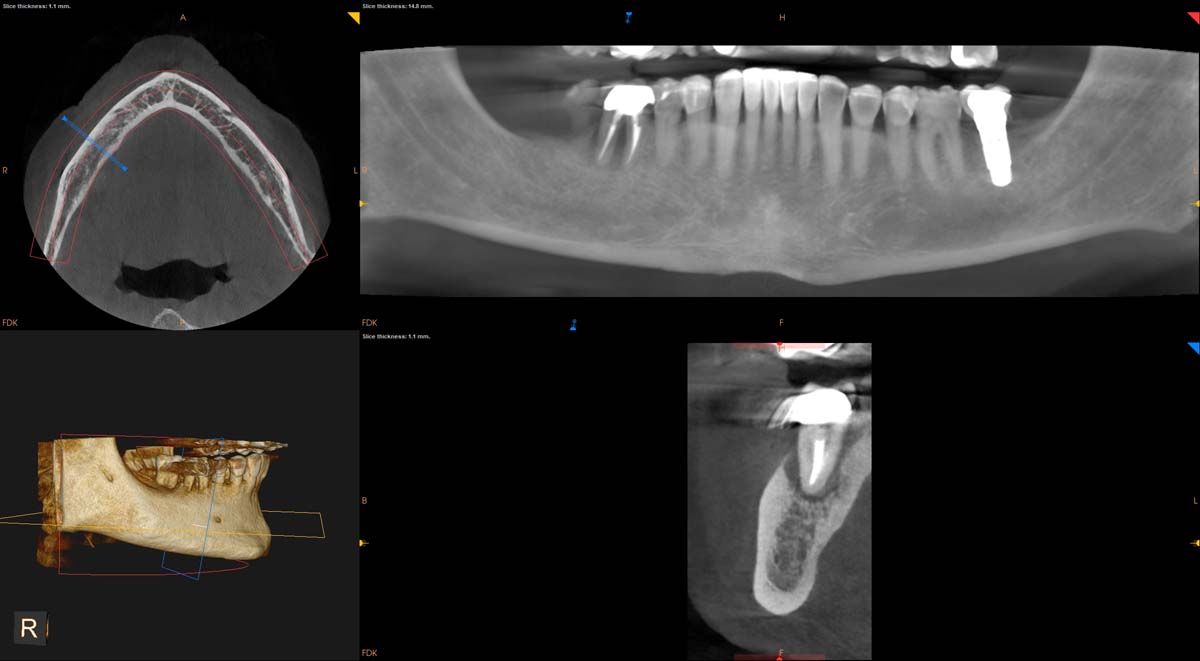
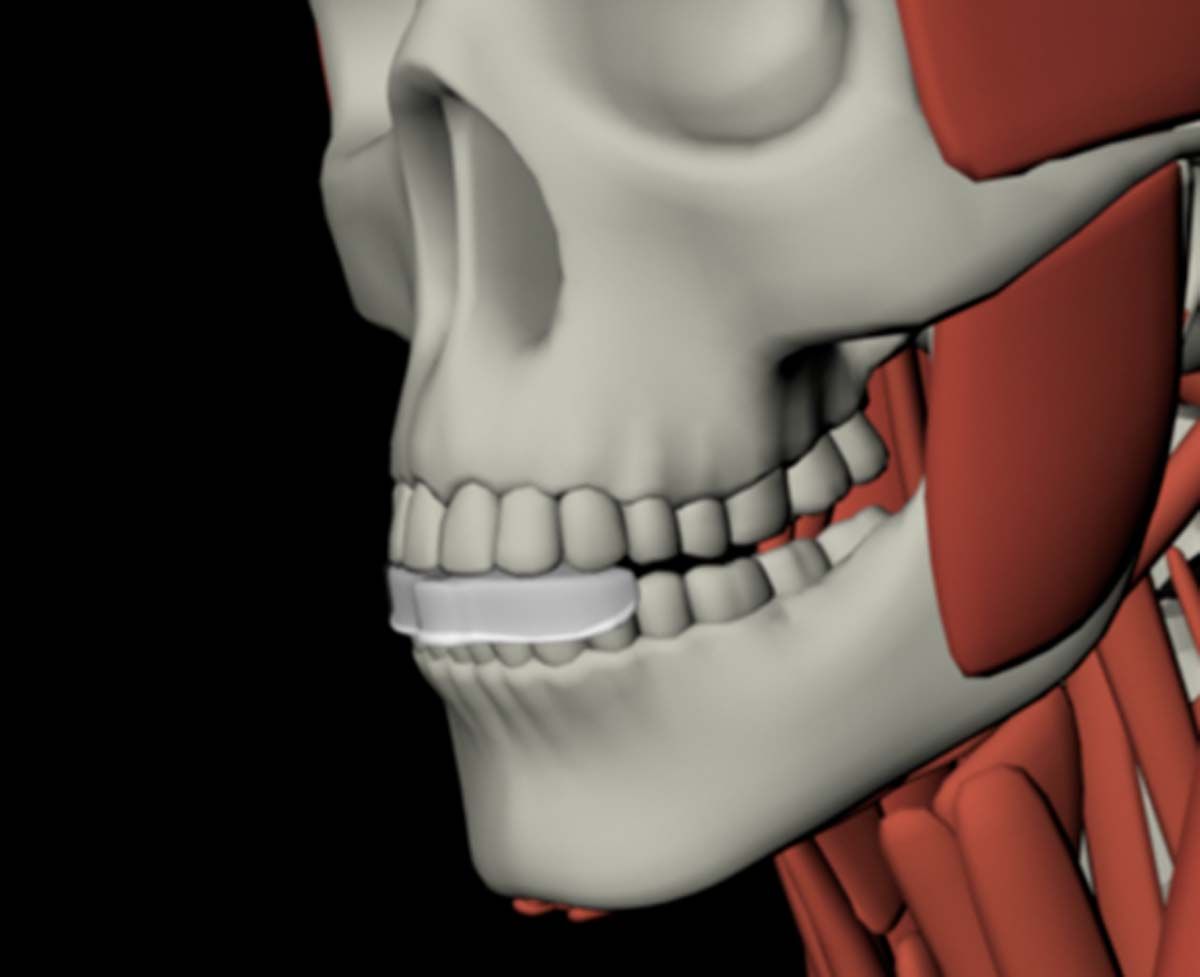
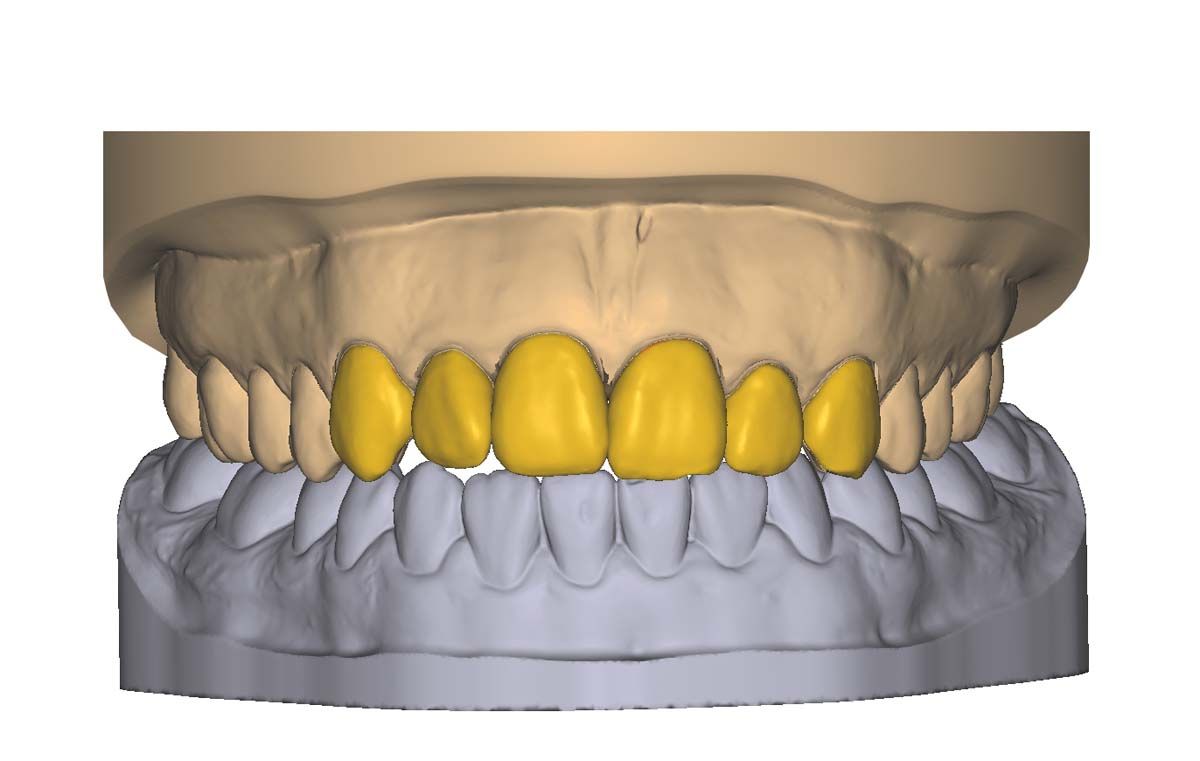
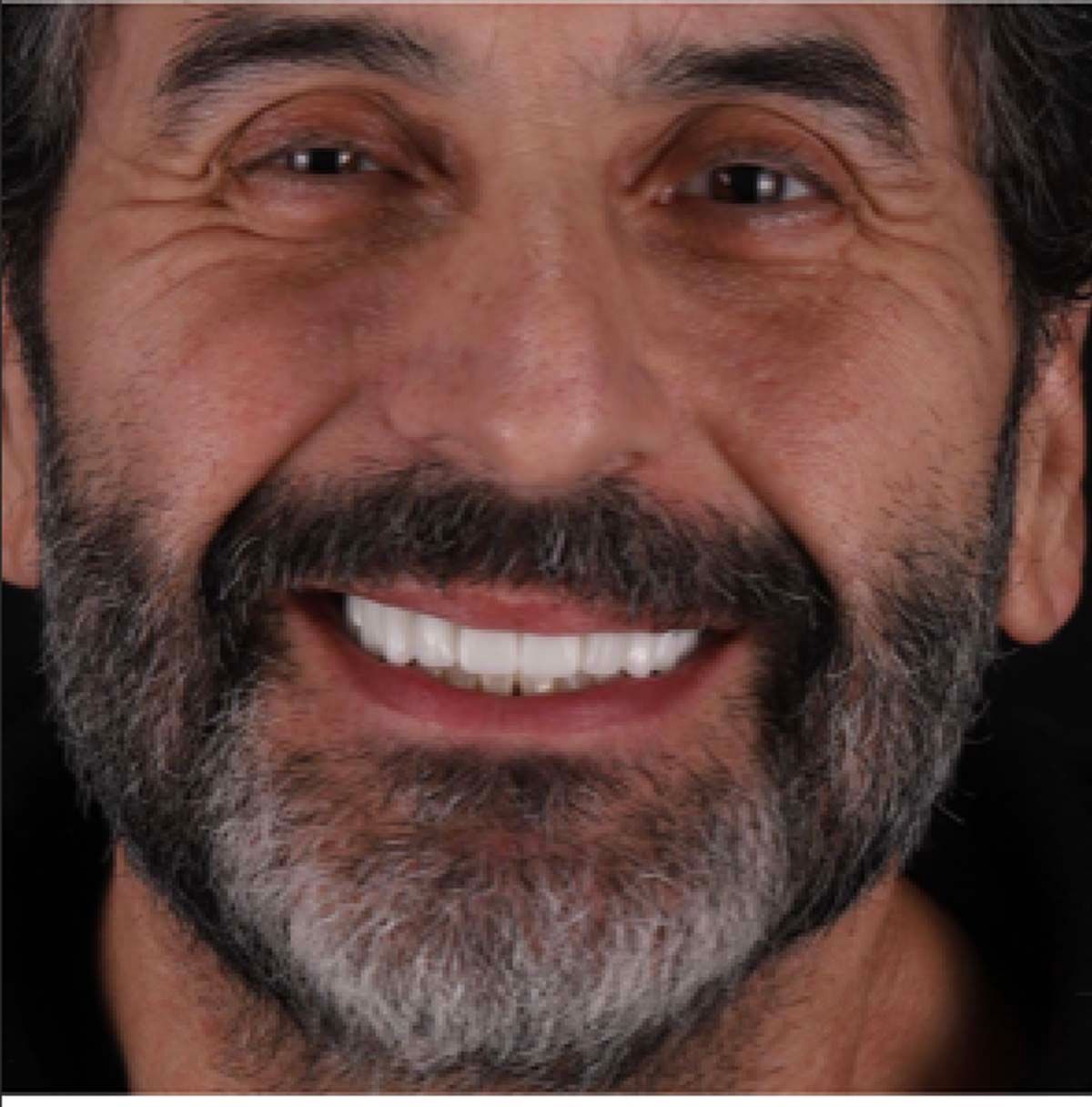
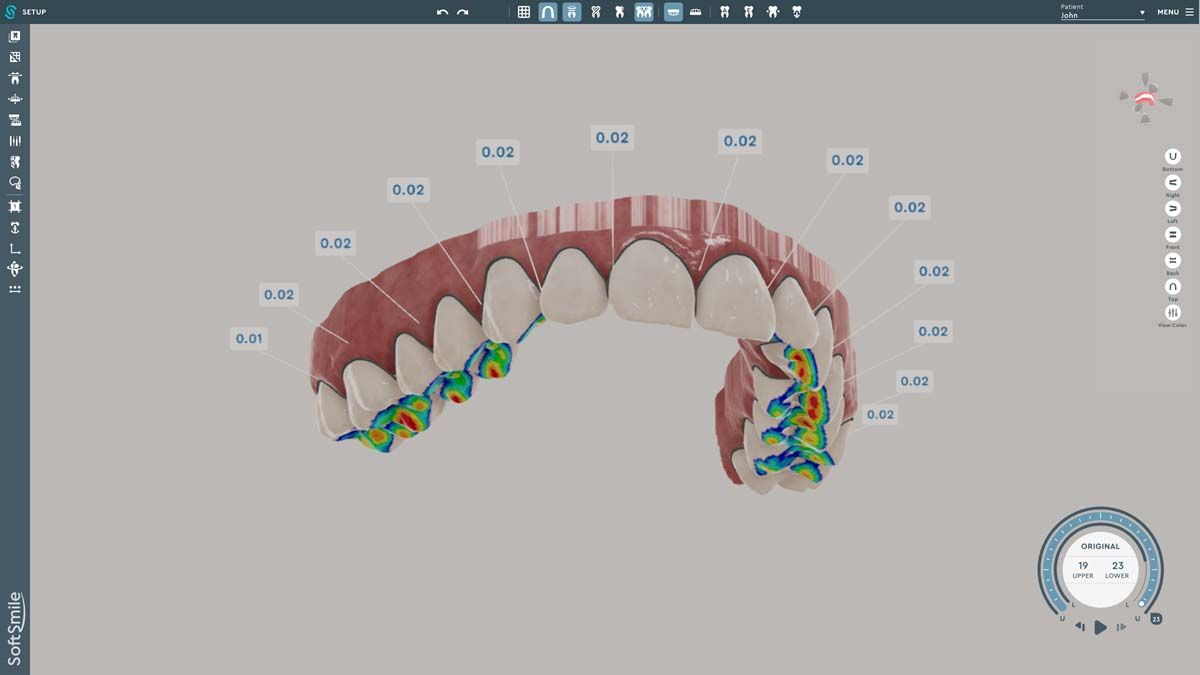
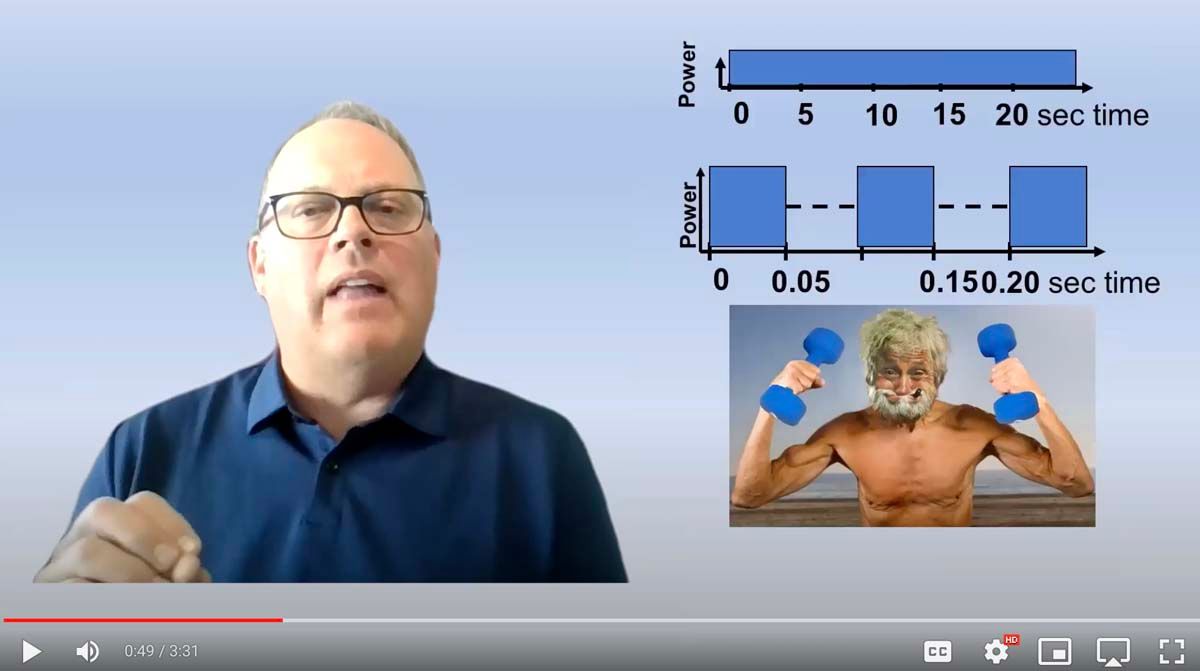
We used to try showing patients their clinical situation on 2D x-rays and demonstrating treatment using models. Later, digital intraoral cameras helped, but they could not show much more than what a patient could see in a mirror. Today, it is possible to show patients every angle of their clinical situation in hyperrealistic 3D with a CBCT scan. Now, when I recommend treatment to patients and they ask why, I am armed with an interactive image captured by my CS 8200 3D extraoral imaging system (Carestream Dental). I scroll through the tooth and bone, point out lesions below the surface, and show why there is or is not enough bone for an implant. If you use something like the Prosthetic-Driven Implant Planning module to automatically merge an intraoral scanner file with the CBCT scan, you create an even more accurate picture. How much easier is it for the patient to accept treatment when they are seeing the end results of that treatment?
Prepare Your Patients
Suppose CBCT has revealed that the issue your patient is experiencing requires a specialist. A 3D scan tells me when it is best to refer treatment, but that can be frustrating and confusing to a patient who was not expecting a second appointment at another office. In that case, the 3D scan lets me prepare patients for the next steps. Yes, they are being sent to a specialist, but they will have realistic expectations about what the next doctor might find and recommend for treatment. Because I also send the scan to the specialist, there are no surprises for anybody; patients do not feel like they are arriving at another office only to be blindsided.
Give Peace of Mind
Oral health care is a negative-demand business. We are telling patients things they do not want to hear. Time, money, and often patient discomfort are involved. You never want a patient leaving your practice wondering what they just agreed to—or, even worse, declining the right treatment because a 2D panoramic image did not look “that bad.” When you use a CBCT system to diagnose, plan treatment, and inform patients about their care, they do not only have confidence in their decision to accept treatment; they have more confidence in you.
Informed consent is more than a patient signing a document, and it is our job as practitioners to provide patients with as much diagnostic information as possible to make that informed decision. When patients feel like they have all the information needed to understand why I am recommending a certain path forward, I know I have done my job.





















 Download Issue: Dental Products Report June 2023
Download Issue: Dental Products Report June 2023

