The creation of an ideally prepared tooth and its detail being “captured” in a master impression are critical steps in the indirect dental restorative process. All can be for naught if a meticulous delivery technique is not followed. Most indirect definitive restorations are crafted with precision on carefully trimmed dies machined with pin placement to align the cast’s preparations in the exact position relative to one another as they appear in the patient’s oral cavity. The final test of accuracy, however, is in the patient’s mouth. Often, ceramic restorations may appear to have perfect fit contact on the master dies relative to one another yet requires adjustment when tried on a patient. Required adjustments are to be expected from time to time when dealing with an indirect fabrication method.
It is also true that multiple adjacent restorations may appear to have proximal contact upon try-on, only to have a slightly altered fit after cementation. Alterations may require a remake if the restoration is placed in an improper position, and it cannot be recovered before the set of the cement. Some clinicians espouse a “multiple cementation technique,” placing 8 to 10 restorations at one time. This can often lead to a disastrous result if even one restoration is placed in a slightly altered position affecting the correct seating of the remaining units.
Dental Cements—A Historical Perspective
By definition, dental cements are “luting agents” meant to fill the microscopic gap between restorative materials and tooth structure. There are multiple types of cement agents.
While universally used for many years, zinc phosphate cements are soluble in oral fluids and can “wash out” when restorative materials are not engineered to fit precisely. Polycarboxylate cements have a slight advantage in that they “chelate” to dentin. Still, the film thickness is greater than that of zinc phosphate cements, which can sometimes be problematic with a fully restored seating. Glass ionomer cements offer some distinct advantages over both zinc phosphates and polycarboxylates. The film is extremely thin, and the material has a fluoride release that has shown to be anticariogenic. The downside? Glass ionomers are still quite soluble in oral fluids.
The next generation in cement evolution moved on to modified resin ionomers. These cements have the advantages of glass ionomers but are even less soluble in the oral environment. In fact, some manufacturers report “zero” solubility with resin ionomers.
A common thread with all of these types of cements is they do not bond to restorative materials. However, the resin cement family evolved out of total-etch and dentin adhesive technologies. Resin cements require pretreatment of the tooth surface with 37% phosphoric acid and the application of a dentin bonding agent prior to application. Resin cements form a micromechanical bond to both tooth structure on one side and restorative material on the other side. Also, they are insoluble in oral fluids.
The latest advance in resin cements is “universal” self-etching cements that may be used with or without a dentin adhesive. They appear to have many advantages of total-etch resin cement systems, yet have the ease of using more traditional types of cements. It is important to emphasize, in some cases, bond strengths of universal self-etching resin cements are not as high when used in “self-etch mode” as those for resin cements using the “total-etch technique” in conjunction with a dentin adhesive. Ideally, it would be beneficial to have a universal adhesive that does not require acid etching to reach optimal bond strengths in enamel and not require light curing prior to cementation, affecting the final marginal fit of the restoration.
It is important to remember that the purpose of any cement is to fill the microgap between tooth structure and restorative material to aid in retaining that restoration. Proper resistance and retention form of preparation is still critical for the successful retention of any restorative material.
Using a Truly Universal Bonding System With Indirect Restorations
Choosing to bond ceramic restorations using a resin cement and dentin adhesive offers one of the higher, if not the highest, bond strength to affix a ceramic restoration to tooth structure. In some clinical situations where maximum bond strength is required, such as for partial coverage ceramic restorations, like porcelain veneers, or for full coverage with less than ideal preparations as far as retentive qualities, it is the method of choice for most clinicians. Still, as with any indirect bonding procedure, there is a degree of technique sensitivity due to the number of steps required to achieve ideal bonding in an environment that can be difficult to isolate from moisture.
Universal bonding systems have simplified the bonding of indirect ceramic restorations. For instance, Tokuyama Universal Bond by Tokuyama Dental America has been introduced with unique features such as no longer needing to light cure the adhesive after application. Also, Tokuyama Universal Bond is a self-curing bonding agent, so it will cure on its own when light cannot reach the material, for example, when bonding zirconium restorations. Another feature of Tokuyama Universal Bond is that there is no need to agitate for 20 seconds to ensure the bonding agent’s penetration into the tooth substrate. Just place, air thin, and cement. Finally, Tokuyama Universal Bond contains primers in both of its components. These included primers mean a separate silane primer is not necessary when bonding glass-ceramics. Even when cementing a zirconium restoration, a separate metallic zirconium primer is also not needed.
A view of the mandibular IPS e.max, from Ivoclar Vivadent, ceramic restorations on the master model before cementation.
Each restoration is etched with 9% hydrofluoric acid (HF) from BISCO for 30 seconds.
The HF etchant is rinsed thoroughly from the inside of the restorations, then air-dried.
Phosphoric acid etch such as Ultra-Etch from Ultradent Products, is placed on the preparations and after 15 seconds is rinsed off with water for at least another 15 seconds. Next, the preparations are thoroughly air-dried.
Consepsis 2% chlorhexidine solution from Ultradent, is used to disinfect the preparation.
The excess chlorhexidine is removed using a high-volume suction so the tooth structure remains hydrated.
The Tokuyama Universal Bond is applied to the preparations.
The bonding agent is air thinned, which evaporates the solvent.
After placing a coat of Tokuyama Universal Bond on the inside of the restoration, it is loaded with resin cement EsteCem II from Tokuyama Dental America.
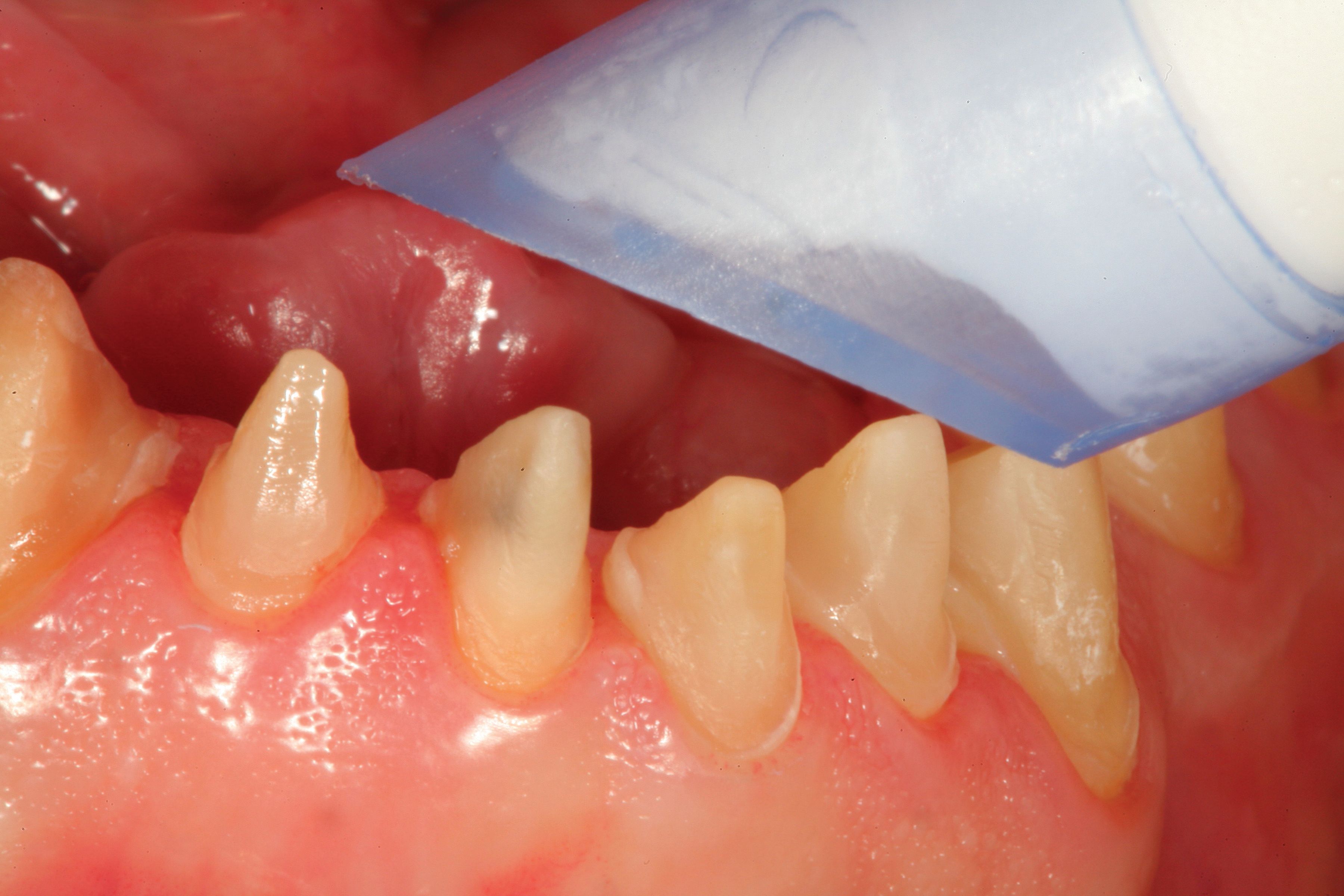
The mandibular incisor restorations are being held in place.
A No. 2 Keystone flat brush from Patterson Dental is bent at a 45-degree angle using a hemostat, then used to remove excess cement from the marginal areas of the seated restoration.
The restorations are tacked to place with a curing light so the remaining excess cement can be cleaned away without dislodging the restorations.
Dental tape is used to remove cement excess from the interproximal areas.
Once cement removal is complete, the restorations are light cured according to the manufacturer’s instructions.
Here is a facial retracted view of the cemented mandibular ceramic restorations.
Here, a protrusive excursion shows separation of all posterior teeth.
In this photo, a right lateral working excursion shows separation of all posterior teeth on the patient’s right side.
In this photo, a left lateral excursion shows separation of all posterior teeth on the patient’s left side. Note that because of the post orthodontic positions of the teeth, the cuspids do not line up. Anterior coupling of the remaining anterior teeth protects the posterior teeth during the functional movement.
This photo features a retracted full arch view of the completed cementation in centric occlusion.
Here, a retracted full arch view of the completed cementation in centric occlusion at a 1-year postoperative visit.
Using a Truly Universal Bonding System—A Case Report
For any multiple-unit cases involving the anterior region, the central and lateral incisors are the most important both esthetically and functionally in guiding the mandible into a protrusive posterior disclusion when the patient’s jaw moves forward during the chewing stroke. The cuspids are also critical as they guide the mandible to separate the posterior teeth during lateral excursions.
Together, these teeth perform a function called “anterior coupling,” allowing all posterior teeth to separate immediately from the centric relation/occlusion position. First, all restorations were tried on individually and evaluated for marginal integrity and fit. Next, proximal contacts were evaluated with dental floss while the dental assistant stabilized adjacent restorations. At this point, proximal contacts should be adjusted with porcelain polishing wheels as needed.
Next, we evaluated the “collective fit” by placing all restorations on their respective preparations and assessing whether the restorations fit passively. Any minor displacement of individual restorations or resistance to complete seating is indicative of a contact that is too tight and needs an adjustment. To make this process easier, we replaced the restoration on the master die in the appropriate position on the master model.
We placed a piece of articulation paper between the restorations to mark the contact area, then “erased” the spot with the porcelain adjuster and reevaluated the fit. This process may need to be repeated a few times before the fit is passive, yet the contact is maintained as “lightly resistant” to dental floss. It is important to note this alone does not mean the restorations will fit passively in the mouth. Remember, teeth don’t move, but dies can move a bit on the master model even when they are pinned.
A facebow transfer and centric occlusion records were taken at the master impression appointment between the maxillary and mandibular preparations. The maxillary provisional restorations and mandibular preparations permit the laboratory technician to “cross mount” the provisional casts and the master casts during the fabrication process. Cross mounting allows for a very accurate approximation in centric relation/occlusion of the definitive maxillary restorations to the mandibular provisional restorations.
Because of this, after the maxillary restorations are adjusted for proximal contact and a passive, collective fit is achieved, an entire maxillary case can now be cemented. Mandibular restorations are adjusted to fit the cemented maxillary restorations then polished as may be required prior to cementation.
In the case illustrated, the maxillary restorations have been placed prior to the mandibular restorations. The first step was to place the central and lateral incisors in position and verify the seat again visually and then radiographically. Digital x-rays allowed for the immediate verification of complete seating on the operatory monitor. For this case, total-etch protocol and resin cement were utilized to maximize bond strength because of occlusal considerations and the patient’s history of clenching.
A properly adjusted occlusal guard was fabricated at the end of treatment to help minimize functional stress on the restorations. In this case, a 37% phosphoric acid etch, Ultra-Etch by Ultradent, was placed on the preparations for 15 seconds (Figure 4), thoroughly rinsed off, then dried with air. The dried preparations were disinfected and rewet with Consepsis 2% chlorhexidine gluconate, also from Ultradent (Figure 5). Consepsis has been shown to inhibit the release of matrix metalloproteinase, which can break down the dentin bond over time.
Next, the excess Consepsis was removed with high-volume suction, so the dentin surface was not desiccated (Figure 6). Because the 4 mandibular incisors will be placed simultaneously, 4 drops of Tokuyama Universal Bond’s A-bond and 4 drops of B-bond were placed in a mixing well, mixed with a micro applicator, then applied to the preparations (Figure 7). The adhesive was air thinned for 5 seconds with low air and, after that, 5 seconds of air thinning with stronger air to evaporate the solvent (Figure 8).
A coat of Tokuyama Universal Bond was placed inside the ceramic restorations, air thinned for 10 more seconds, then filled with EsteCem II, Tokuyama Dental America’s resin cement (Figure 9). Tokuyama Universal Bond is an excellent companion product to EsteCem II because it exhibits enhanced bond strengths to all substrates without the necessity of extra activators or primers. This helps simplify the cementation process since the same protocol can be used regardless of the choice of restorative material.
Once both central and lateral incisors are completely seated with positive pressure expressing excess around the periphery of the margins (Figure 10), a No. 2 Keystone brush from Patterson Dental was used to wipe away all excess material (Figure 11). A tacking tip is used to spot cure the restorations in the center to stabilize (Figure 12) while continuing cement clean up with the sable brush, and then dental tape was applied (Figure 13).
The final cure of all restorations was completed according to the manufacturer’s instructions (Figure 14). There is now a retracted facial view of the central and lateral incisors after placement (Figure 15). This process was completed respectively for the cuspids and first premolars, leaving only the first molars to cement next to the natural remaining second molars.
Invariably at this point, even though there may have been a passive fit before, these restorations may now be tight and not go to full seat. Proximal contacts should be marked with articulation paper on the master model, as previously described, then adjusted and checked with dental floss in the patient’s mouth. When the first molar restorations have a passive, full seat, they can be cemented.
The patient was instructed to close into light occlusal contact on Parkell’s AccuFilm II articulating paper. One of 3 possibilities will occur: the patient will contact and mark only on the occlusal surface(s) of one or both of the posterior teeth, the patient will contact only on the incisal edges of the mandibular incisors, or there will be simultaneous contact on both posterior units and the mandibular incisor restorations.
If one or both posterior units contact first, the centric prematurity, or prematurities, are identified and adjusted using a red stripe 30-micron composite finishing diamond from Komet USA and rechecked with AccuFilm until simultaneous contact on both anterior units and posterior units were achieved. If the anterior units contact first, either the incisal edges need shortening, or the maxillary lingual concavities of the maxillary central incisors need deepening. Again, the goal is to achieve simultaneous, even closure with all of these units in place.
It is important to think of occlusal stability like a “3-legged stool.” One can sit on a 3-legged stool very easily but cut one leg off, and it gets harder to balance. Muscles are activated to maintain a stable seating position that may have been at rest before. What does this have to do with restorations? The minimal contact for a stable occlusion is a contact with the maxillary and mandibular central incisors and a posterior contact, as far posterior as possible, on each side.
This does not mean that the occlusion is considered stable with only 3 points of contact, but it’s a start. The ultimate goal is to have even and simultaneous contact of all maxillary and mandibular teeth in centric relation/occlusion (maximum intercuspation). Posterior teeth should touch only in centric relation/occlusion. Any movement from that position, such as working, balancing, and protrusive position, should result in immediate disclusion of all posterior teeth because of canine guidance and anterior coupling (Figures 16-18).
Ready for Any Cementation Scenario
A technique has been described for methodical and predictable cementation of multiunit ceramic dental reconstruction. A 1-year, postoperative view of the completed case is shown in Figures 19 and 20. This technique can be applied to any cementation plan, regardless of the number of units involved. It should also be mentioned that it is very important to verify final cementation with digital bitewing radiographs to ensure accuracy and complete cement removal.




















 Download Issue: Dental Products Report October 2020
Download Issue: Dental Products Report October 2020

