How to Treatment Sequence Both Arches With In-Office Virtual Planning and Provisionalization
It can be a challenge to treat both arches with implants. But proper treatment planning and sequencing can help.
Treating both arches with implants following extraction of the existing dentition can create challenges for the practitioner. Virtual planning and treatment sequencing can allow for fewer potential issues on the way to the desired result. Utilization of virtual planning with 3D printing of surgical guides and immediate provisional restorations simplifies the chairside aspect of treatment. Additionally, the 3D-printed provisional restorations allows the patient to test the esthetics and function to permit patient input into the design of the final restorations. The case discussed follows a challenging case and the virtual planning and execution to achieve the patient’s desired result.
Introduction
Treating both arches can be a challenging endeavor when the maxilla and mandible present with failing dentition. Treatment sequencing allows the practitioner to better plan the procedures with the end result being a screw retained provisional hybrid prosthesis on both arches. This allows the patient something comfortable to utilize during the osseointegration period before the final prosthesis is fabricated. Additionally, the provisional prosthesis can be looked on as a “test drive” of what the final prosthesis will look and feel like, allowing changes based on the patient’s feedback.
Case Presentation
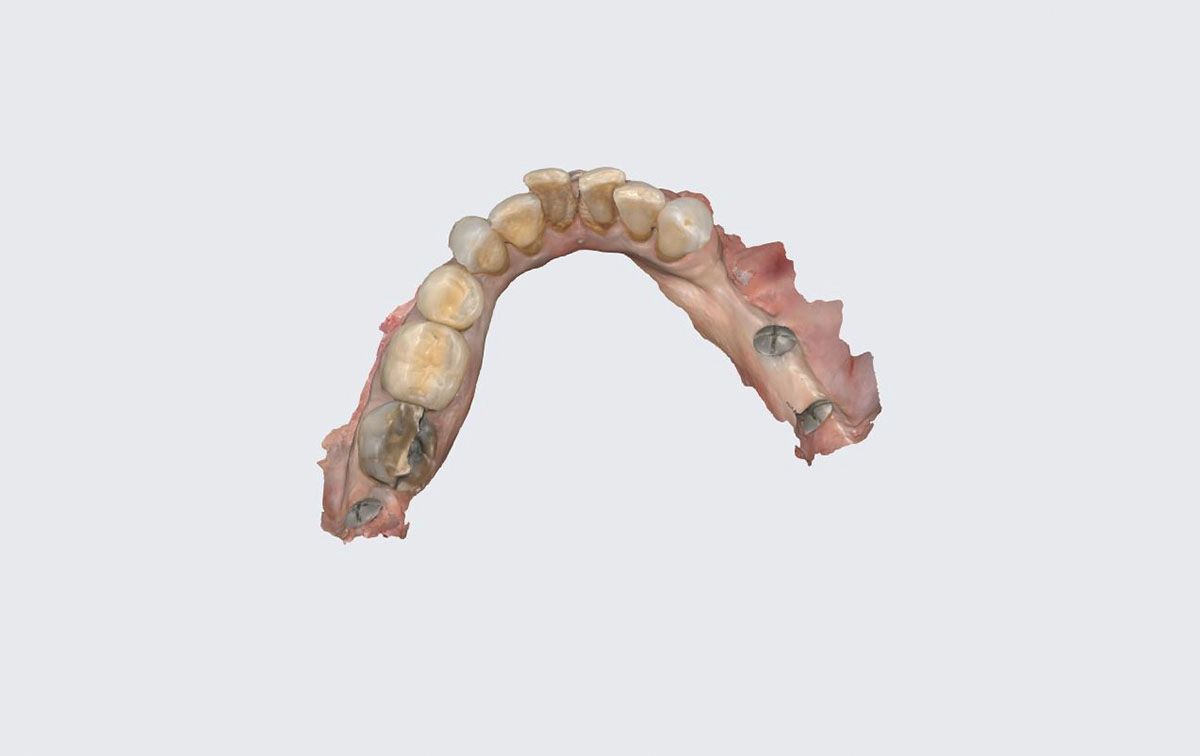
A 67-year-old woman presented for consultation expressing issues with the esthetics of her smile and discomfort with the remaining dentition (Figure 1). The patient had been seen prior in the practice 11 years prior. A panoramic radiograph was taken to evaluate the remaining dentition, osseous structures of the arches, and the available anatomy that could accommodate implant placement selected as a treatment (Figure 2). Generalized bleeding with mobility on the remaining dentition of the maxilla and posterior left mandible of grade 2 or greater was noted. The patient was informed that the dentition had severe issues and treatment could not be performed to salvage those teeth. The patient was informed that traditional full dentures could be fabricated, or implants could be placed in both arches and a fixed hybrid prosthesis used to restore both arches. The patient preferred the implant fixed prosthetic option.
The treatment staging would be to extract the maxillary teeth, place those implants and an immediate screw retained provisional prosthesis if insertion torque was achieved of 35 Ncm or greater. The patient would then return and have a similar approach performed on the mandibular arch then allowed to heal and test drive the prosthetics during the osseointegration healing period to make any esthetic or tooth position change the patient requested.
Orientation screws were placed into the arches to have a stable marker for the intraoral scan virtual model creation and increase accuracy of the process. The orientation screws were placed on the day of surgery. Once the screws were placed, a pre-op scan was taken, then teeth were extracted, and implants placed. The MUAs and white caps were placed on the implants and the arch was rescanned. The pre-op scan and the post-op scan were then merged using the screws as reference points so that the provision can be designed at the proper VDO. The arches were scanned with an intraoral scanner (Medit i500, Medit Inc,) to initiate the treatment planning.
Virtual Planning for Surgical Guide and Provisional Fabrication
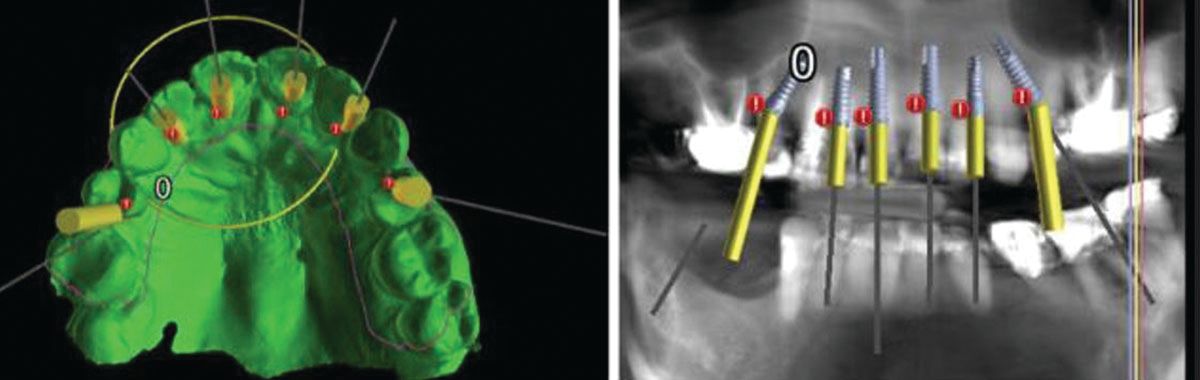
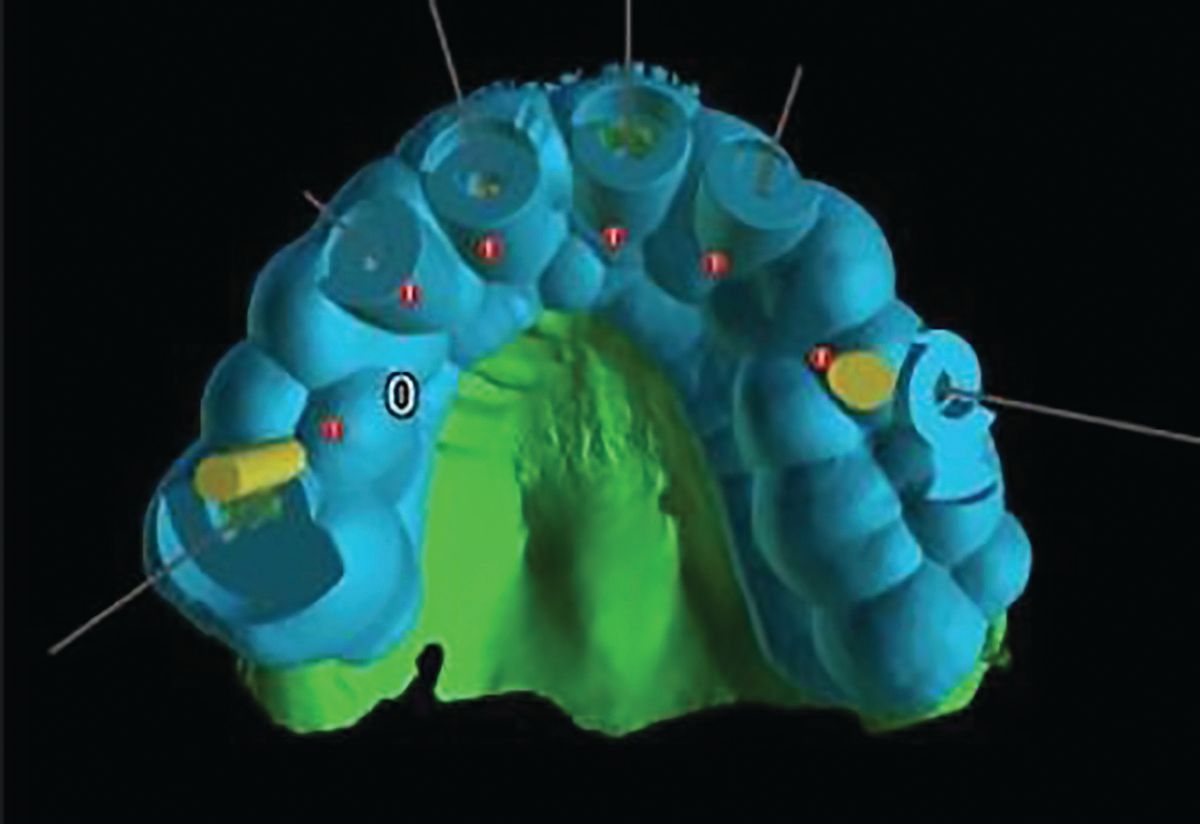
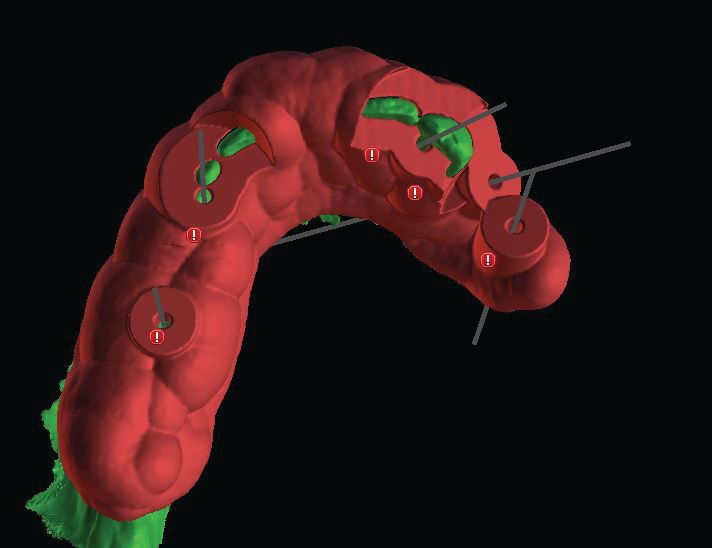
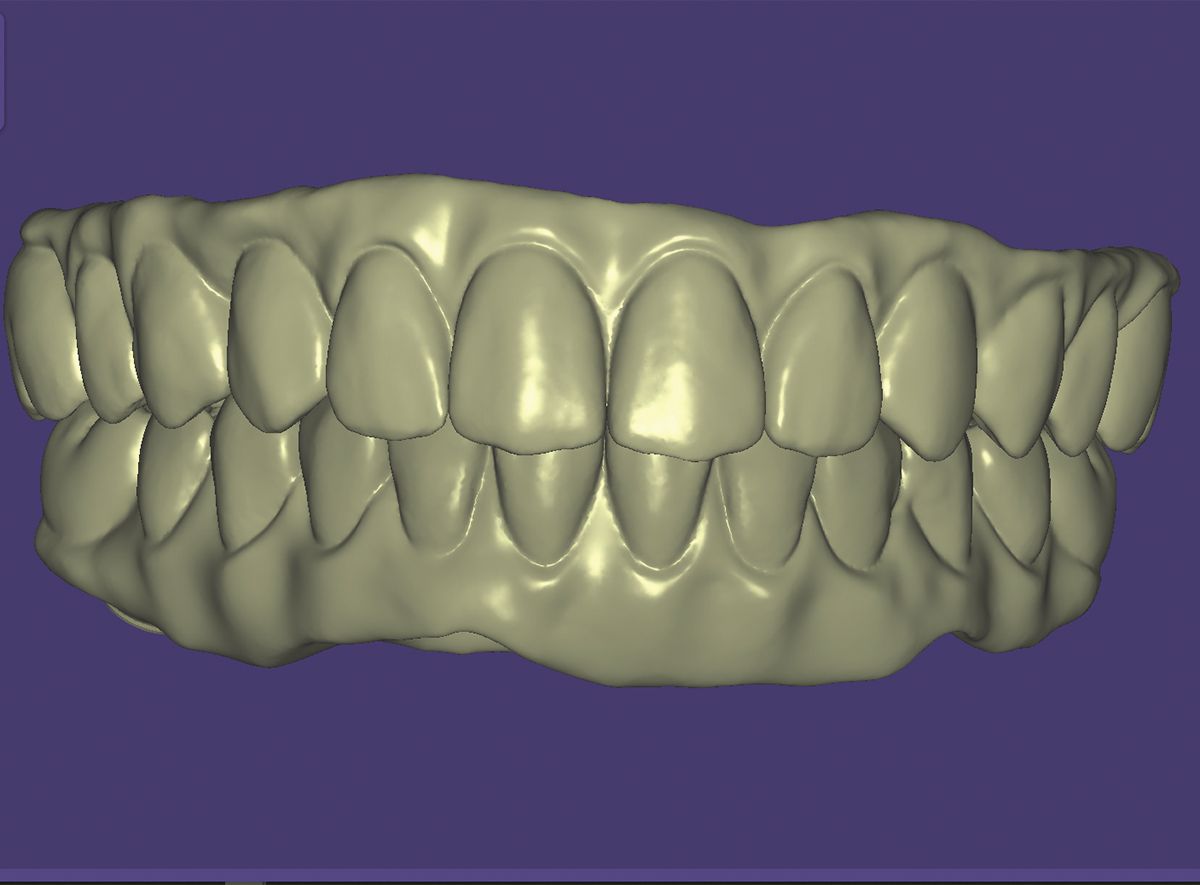
The intraoral scan of the maxillary arch was performed (Figure 3). The scan was imported along with the CBCT scan into BlueSky Plan (BlueSkyBio) and a virtual model was created. Based on the anatomy present, implants were virtually placed on the CBCT scan (Figure 4a), and emergence of the implants were verified in relation to the teeth to position the screw access in a non-esthetic position (Figure 4b). The software was then utilized to design a surgical guide for the maxillary arch to guide implant placement. (Figure 5) This would permit prefabrication of an immediate screw retained provisional restoration to be placed at the placement appointment.
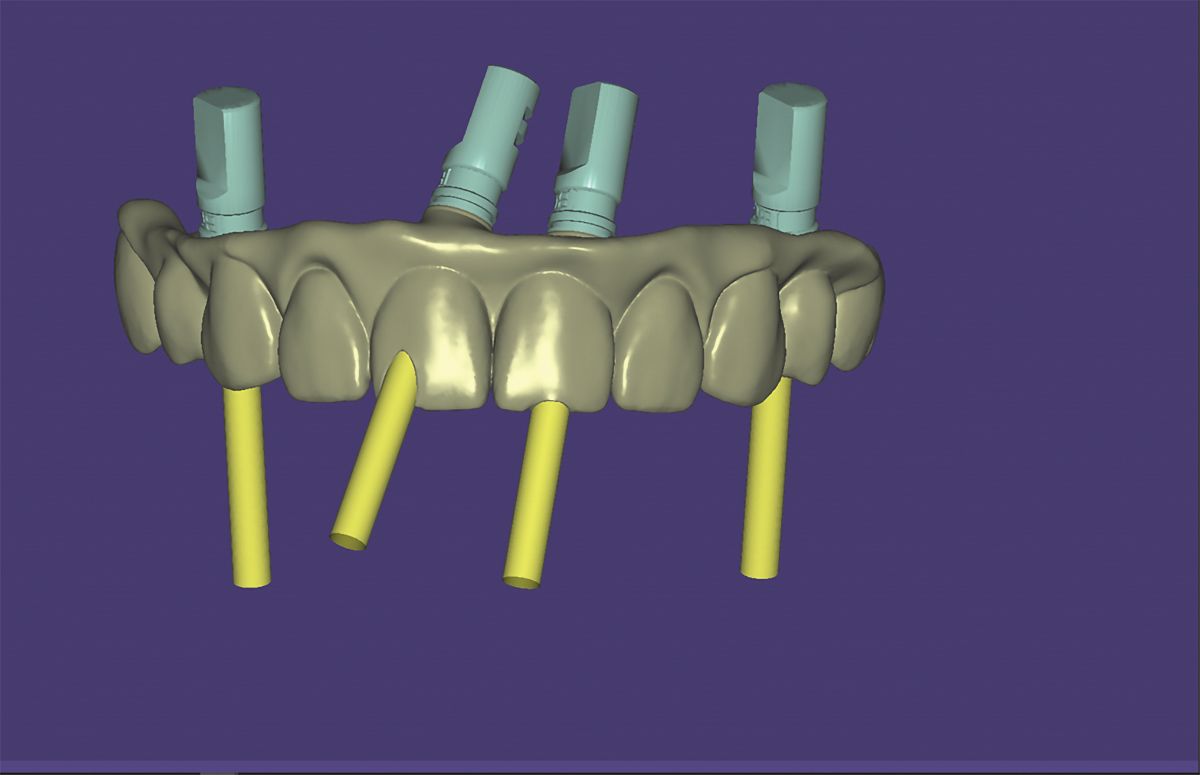
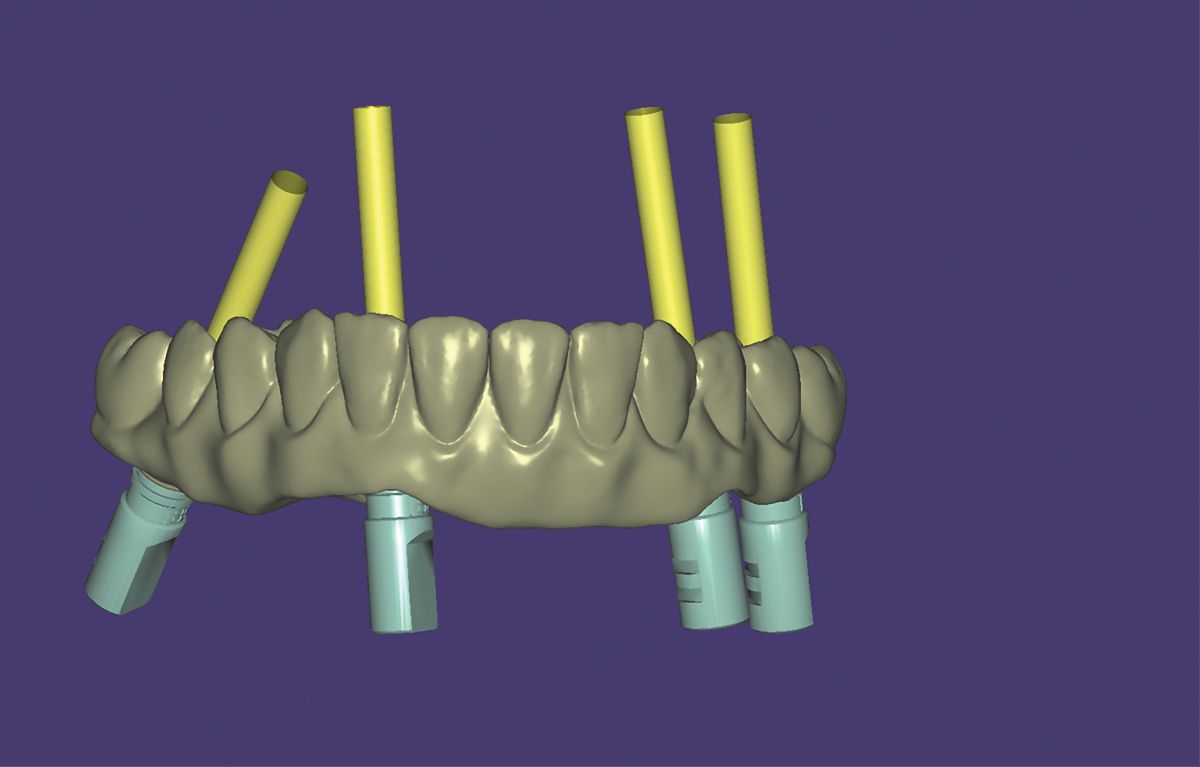
The teeth were removed on the virtual maxillary arch and replaced with a digital wax up of the full arch prosthesis based on the planned implant position(Figure 6). The model was then removed virtually leaving the implants and their trajectory through the planned provisional screw retained restoration to verify screw access (Figure 7).
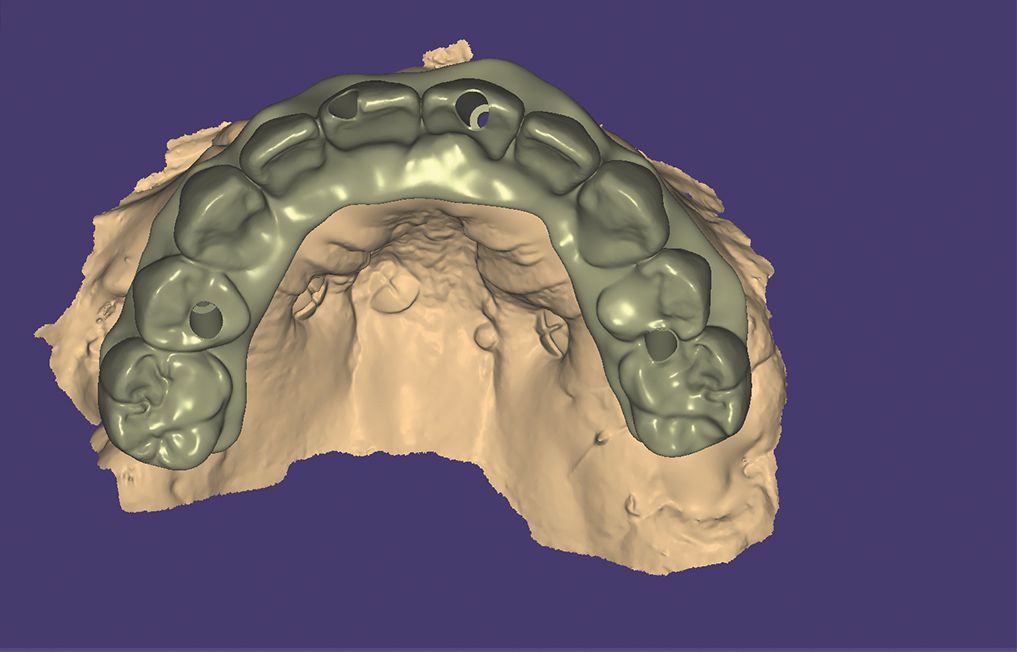
The intraoral scan of the mandibular arch was performed (Figure 8). This was imported into BlueSky Plan to virtually plan implant placement, surgical guide, and immediate provisional prosthesis fabrication. This was performed in a similar matter in the software as had just been performed for the maxillary arch. (Figures 9, 10, and 11) Implants would be placed with anticipation of achieving adequate torque values that would allow immediate loading with a fixed provisional.
Being unable to immediately load that arch due to insufficient insertion torque remained a potential, and a provisional full arch denture was planned. The denture was virtually designed with the teeth being positioned to be in occlusion with the virtual designed maxillary screw retained provisional restoration (Figure 12). A full mandibular denture was printed.
Maxilla: Implant Placement and Immediate Provisionalization
The patient presented and was instructed to swish with a 0.12% chlorhexidine oral rinse to reduce oral bacteria prior to initiation of the surgical treatment at the appointment. Local anesthetic was administered as infiltration into the buccal vestibule from tuberosity to tuberosity and on the palatal surface. The maxillary remaining dentition was atraumatically extracted using elevators to luxate the teeth and then by use of forceps.
The surgical guide (Figure 13) was inserted, and osteotomies created for the 6 planned implants in the maxillary arch. Implants (ULT, Ditron) were placed at site #4, #5, #8, #9, #11, and #14. The ULT implant was selected due to its reverse concave neck, allowing platform switching and thicker bone at the crestal portion of the implant for long-term maintenance. Insertion torque was greater than 35 Ncm at all implants except #5 and it was decided to not immediately load that implant with the provisional hybrid restoration being supported by the other 5 implants. A cover screw was placed into implant #5. Following implant placement, multiunit abutments (MUA) (Ditron) were placed on the implants. MUA were placed on the implants to aid in placing the screw access opening on the planned prosthetics either on the lingual (anterior implants) or occlusal surfaces (posterior implants). White caps were then placed on the MUA, and the arch was scanned intraorally.
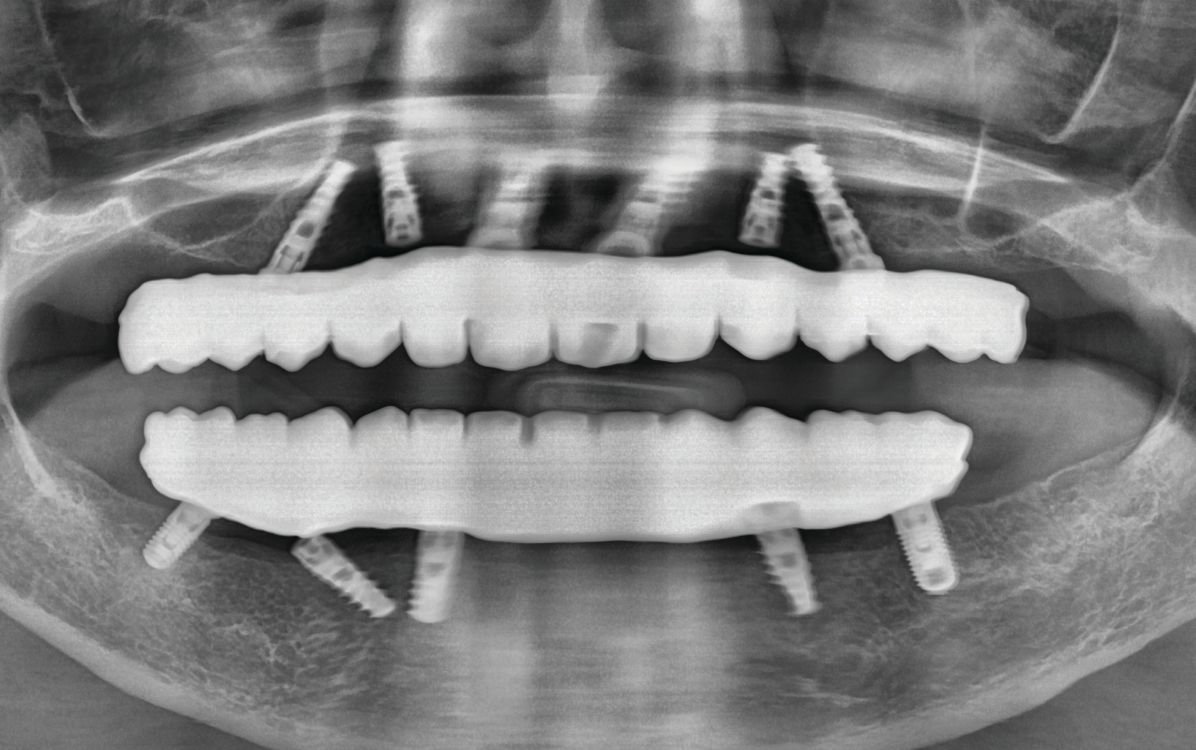
OraGRAFT, (LifeNet Health) was placed into the extraction sockets not occupied by implants and a piece of Collagen Patch (Zimmer Biomet) was placed over those sockets and fixated with a 4-0 PDA suture to contain the graft during healing while soft tissue closure progressed. The previously 3D printed screw retained provisional restoration was inserted intraorally to verify seating and the screw was tightened to finger tightness on implants #4, #8, #9, #11, and #14. A panoramic radiograph was taken to verify complete mating of the tibase in the provisional restoration and implants (Figure 14). A piece of PTFE tape was placed into each screw access hole and the hole was sealed with Premise Flowable composite (Kerr Dental). Occlusion was checked and adjusted on the mandibular arch where needed to have uniform occlusion. The position of the teeth in the maxillary provisional mimicked the position of the natural teeth and the midline following the natural teeth was to the right of the patient’s facial midline (Figure 15).
Virtual design has some challenges as the facial anatomy are not present, so identification of the facial midline cannot be appreciated. In this case, the midline followed the midline of the teeth present which, was to the right of the patient’s facial midline. This would be corrected with a subsequent provisional when the mandibular arch was treated after allowing the maxilla to heal for 4-6 weeks. Sutures were removed at 4 weeks post-surgery.
The patient returned at 4 weeks post treatment of the maxilla to initiate treatment of the mandibular arch. The mandibular arch was treated in a similar surgical protocol as the maxilla.
Due to the stability of the mandibular implants, it was decided to not immediately load the mandibular arch. Cover screws were placed into the implants. MUA were placed on the implants to aid in placing the screw access opening on the planned prosthetics either on the lingual (anterior implants) or occlusal surfaces (posterior implants). The following angulations with the MUA were placed in the mandibular implants were straight (00). White caps were then placed on the MUA, and the arch was scanned intraorally.
OraGRAFT was placed into the extraction sockets not occupied by implants and a piece of collagen membrane placed over those sockets and fixated with a 4-0 PDA suture to contain the graft during healing while soft tissue closure progressed. A digital preprinted mandibular denture was tried in and lined with a soft material, MucoSoft (Parkell). Occlusion was checked and adjusted as needed.
The patient presented at the postoperative appointment 1 week later, indicating she felt she was hitting the posteriors before the anterior teeth in the prosthetics. She also reported the lowers were having difficulty staying on the arch and some minor discomfort on the gingival tissue. The sutures were removed, and the patient instructed to see if that helped the soreness. Patient was scheduled to return in a week to reline the lower denture to help improve comfort and stability.
A week later, the patient presented and upon removal of the provisional denture the soft tissue had improved, and healing was progressing. She indicated the area was tender and small spicules of bone were noted and removed with cotton pliers. The patient was reappointed to allow further healing.
A hard reline of the mandibular denture was accomplished at a subsequent appointment utilizing MucoHard (Parkell). The mandibular implants would be uncovered at 3 months post-surgical placement and a screw retained provisional mandibular prosthesis placed with a new maxillary screw retained provisional prosthesis with shift of the facial midline to the left to improve the esthetics and allow the patient to test drive the new provisionals.
Final Provisionalization of the Maxillary and Mandibular Arches
The patient returned at 3 months post mandibular implant placement and implants were uncovered and healing abutments placed on the mandibular arch. The maxillary provisional hybrid was supported on 5 of the 6 implants that had been placed, during the prior months due to low stability on the implant at site #5 at placement. The patient was informed that this implant and the implant at site #11 could be included in the final prosthesis, but surgery to uncover the implant at site #5 would be necessary. The patient opted to leave that implant as a sleeper to avoid the additional surgery. She was informed should the implant at sites #4 or #8 develop issues, that implant could be added to a new prosthesis in the future. The same decision was made at site #11 in the final prosthesis. In the mandibular arch, it was decided to sleep the implant at #27 as the other 4 implants had high stability following integration and would not be needed to support the planned prosthesis. An intraoral scan was taken to capture the ridge dimensions following implant healing (Figure 16, right) which was imported into BlueSky Plan along with a previous scan of the maxillary arch (Figure 16, left). New screw retained provisional prosthesis on the maxillary and mandibular arches were designed virtually shifting the midline to the left and aligning it on both arches (Figure 17). The provisionals were then printed in Flexcera Smile using an Envision One 3D printer (Desktop Health).
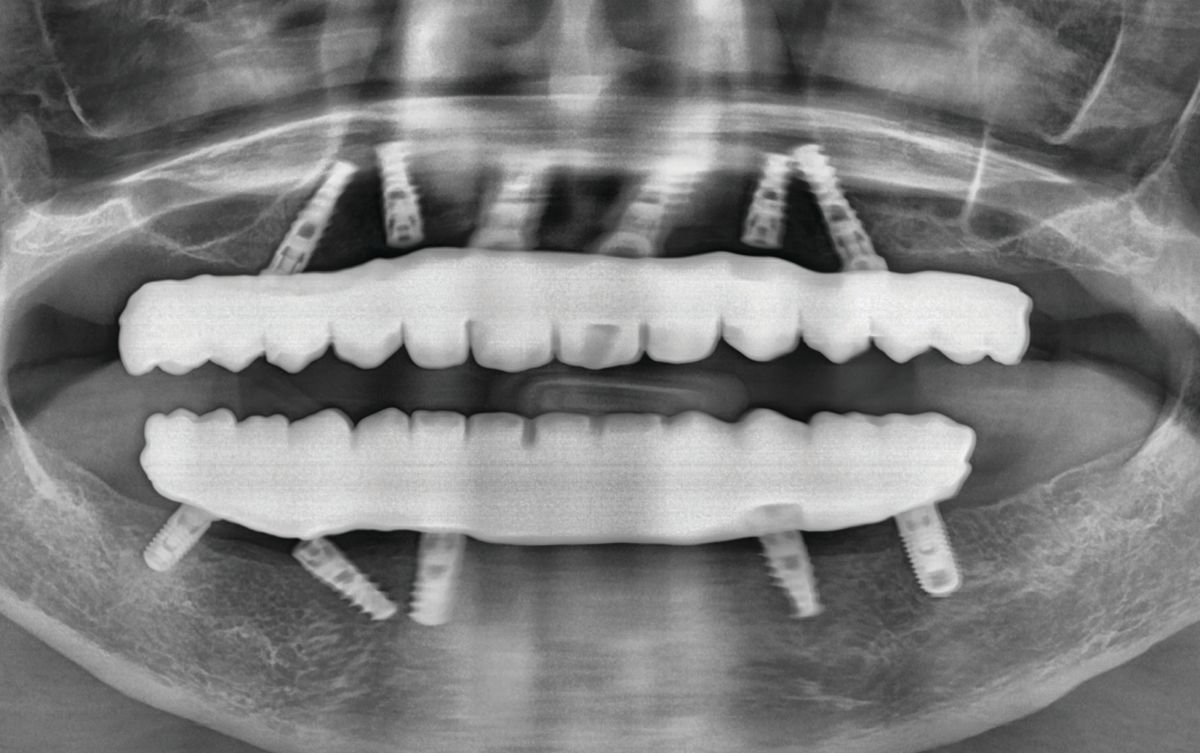
The patient presented and the maxillary screw retained provisional hybrid and mandibular healing abutments were removed. The new maxillary provisional hybrid was inserted intraorally as well as the mandibular provisional hybrid. A panoramic radiograph was taken to confirm complete seating of the provisional hybrid prosthetics with the underlying implants (Figure 18). The patient was shown a mirror and indicated she was happy with the esthetics. Test driving these would allow the patient to see what further esthetic changes are possible.
Finalization of the Final Prosthetics
The patient returned after 2-weeks for final approval on the esthetics of the current provisionals so any desired changes could be communicated to the lab for fabrication of the final restorations. Scan flags (PIC transfers, PIC Dental) were placed onto the MUA’s on the maxillary implants that would be included in the final prosthesis and a scan was done to provide the lab with a digital verification jig to virtually design and fabricate the prosthesis (Figure 20a). This was repeated in the mandibular arch (Figure 20b). The information along with the design file from BlueSky Plan was sent to the lab with a prescription to fabricate screw retained zirconia monolithic hybrid restorations for both arches.
Placement of the Final Restorations
The final prosthetics were returned from the lab and the patient appointed for insertion. The patient presented and the provisional prosthetics were removed intraorally. The maxillary screw retained monolithic zirconia hybrid was inserted and the fixation screws tightened to finger pressure into the MUA on the implants. The mandibular prosthesis was inserted intraorally. A panoramic radiograph was taken to verify complete mating of the prosthetics to the MUA on the implants intraorally (Figure 21). A piece of PTFE tape was placed into each screw access hole and then sealed with composite which was leveled with the surface of the zirconia and light-cured. Occlusion was checked and adjusted where needed.
The patient was shown a mirror and she expressed satisfaction with the final esthetic results (Figure 22). She was scheduled to be seen for a post-insertion appointment at 1 week to check the occlusion adjust as needed.
Conclusion
Implant selection is critical, especially when immediate loading is planned. Aggressive deep threads aid in initial stability of the implant and better insertion torque to allow immediate loading. This, combined with a reverse concave neck and micro threading, allow thicker crestal bone around the implant which will aid in preservation of bone during long-term function and decrease bone loss potential. The Ditron implant was selected, meeting those 2 criteria for use in this case.
Utilization of virtual planning, guided surgery, and 3D printed surgical guides, as well as implant provisional restorations can simplify the treatment process.

















 Download Issue: Dental Products Report August 2022
Download Issue: Dental Products Report August 2022

