How to Become a Class II Smooth Operator
Class II posterior direct restorations often present as complex cases. But Clean & Boost® Dentin and Enamel Cleanser from Vista Apex can increase bond strength while leaving the smear layer intact.
Dentists see all types of direct restorative cases throughout their days, weeks, and years, but the most common is a Class II. With the demand for esthetic composite restorations, clinicians find that complexity in restoring a posterior tooth to its natural appearance and function has only increased.
Study results have shown that dental resin composites have an average life of 5.7 years, with the main causes of failure being secondary decay and fracture of the restoration.1 The factors that contribute to failure are mostly poor adhesion protocols, inadequate interproximal contacts, improper polymerization, and poor placement of materials.
The challenges that dentists must overcome to achieve a desired patient outcome are immense but achievable if we avoid the pitfalls of restorative failure. Here is an outline of some of the most common pitfalls with tips to help practices.
Isolation
In the days of placing amalgam, isolation was not as critical. As we use advanced materials that are more technique-sensitive and don’t work well in a moist or wet field, we must control moisture and bleeding.
Dentists will see more failures if they do not have good isolation in place. Investing in a refresher course on rubber dams or in a device such as DryShield® from DryShield or Isolite from Zyris® will provide benefits that far outweigh any costs. Depending on the procedure and patient, I will use either rubber dam isolation (Figure 1) or DryShield (Figure 2).
Sealing the Gingival Margin
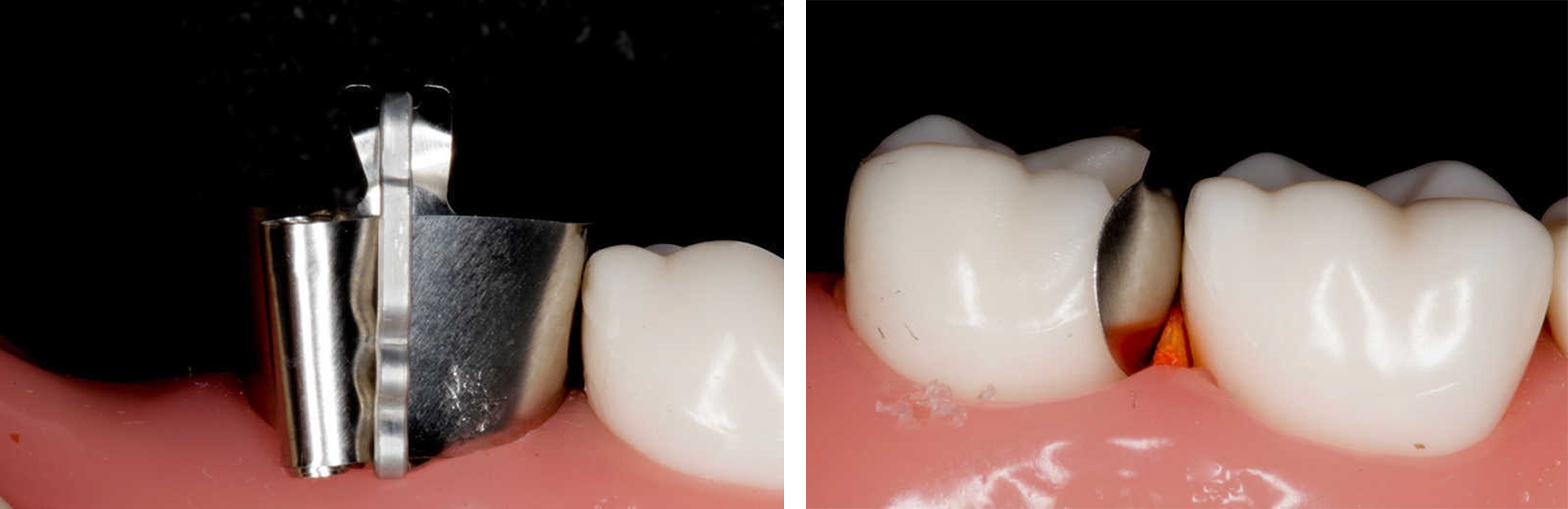
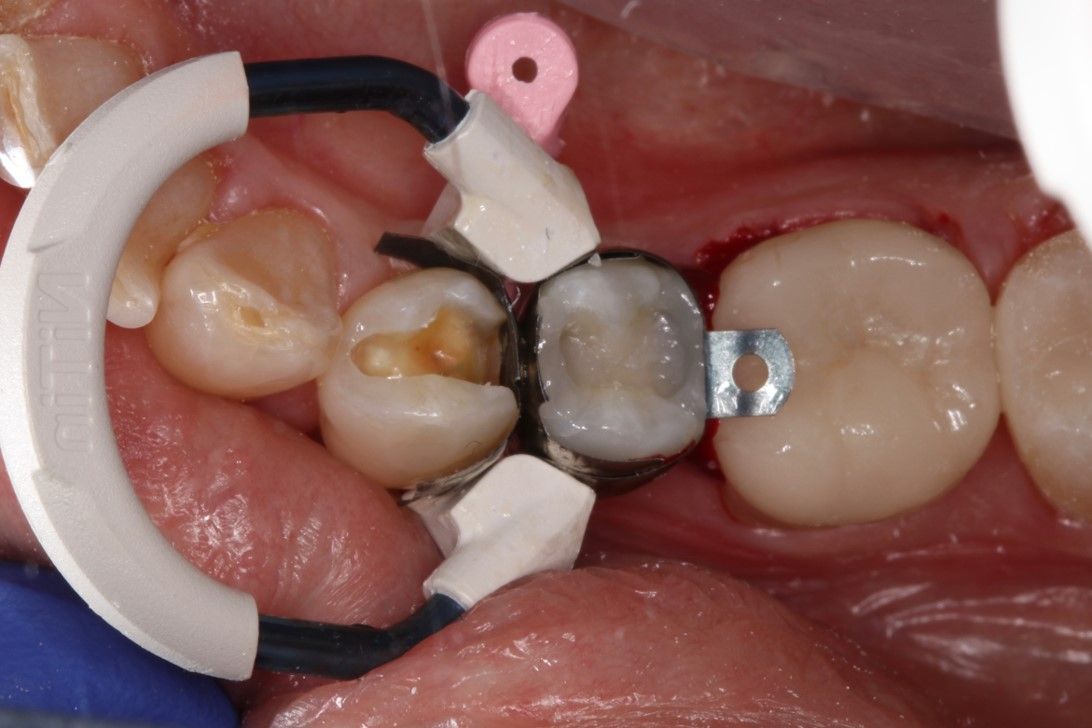
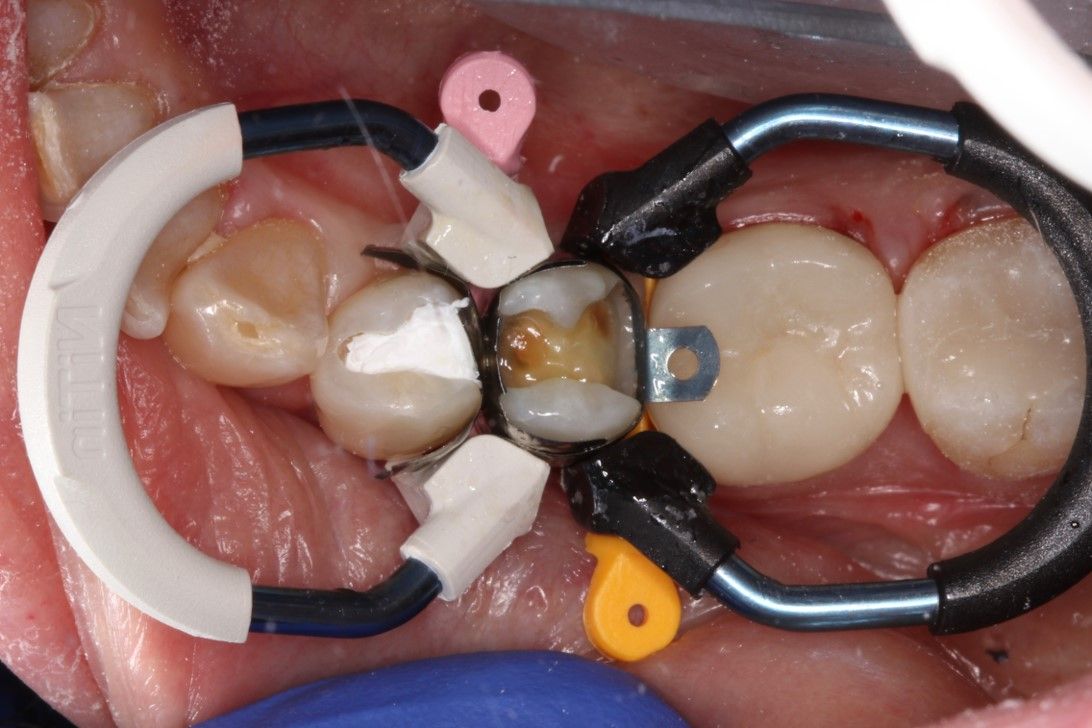
There is an abundance of matrix options, both circumferential (Figure 3) and sectional (Figure 4), to help handle situations with composites, but these options do have their limitations. The components of matrix systems are matrices, wedges, and bands. I use 3 or 4 different sectional systems in my office for different situations.
I typically avoid circumferential matrices because they will drive my contact point to the occlusal surface, taking away the ability to manipulate that circumferential band when packing composite. When I place composite into a very unfavorable physical characteristic, it will fail time and time again regardless of the composite used.
The role of the wedge (Figure 5) in adhesive dentistry is to maintain a gingival seal and allow proper band contour to achieve ideal anatomic contact. The wedge should not negatively impact the shape of the sectional matrix and should not create separation. I prefer plastic wedges, which tend to have a truly anatomic form, protect papilla, and are easy to place under contacts. That said, they are more costly. But what is a smooth operator’s time worth?
Bands come in various options. What is most important is that there is an array of sizes in the office. There should always be 0.5 to 1 mm above the adjacent tooth structure. If it is elevated more than that, it pushes the concavity that creates that ideal contact from mid contact point up to the occlusal embrasure space, much like circumferential matrices.
Clinicians should look for a system that is flexible and allows them to stack. In Figure 6, clinicians can see the Palodent® Plus system from Dentsply Sirona with a nice built-in angulation to its rings, so they go on and stack easily.
The final critical component of being successful with a matrix system is Teflon tape. Clinicians can buy this at any hardware store and should have a roll in every operatory.
Pictured is a mesial-occlusal-distal on the premolar (Figure 7) and a distal occlusal on another premolar (Figure 8). The matrixes are all in place and packed with Teflon tape in the contact point to create a rigid surface, so when I go to the mesial of the second premolar, I can burnish that against something of rigidity.
Another great use of Teflon tape is to minimize buccal and lingual flash, by packing the tape into the buccal lingual gaps that the rings provide (Figure 9). When it’s done, the buccal, lingual polishing and finishing are much easier (Figure 10).
Creating the Ideal Hybrid Layer
Regardless of the adhesive material used, the best advice I can give is always to read the instructions. Clinicians are amazed at the instructional nuances that can cause restorative failures. I am a self-proclaimed self-etcher, and I don’t total-etch unless I am 100% into the enamel.
Although a total-etch technique absolutely works, I prefer self-etch, which I find to be less technique sensitive. Total-etch obliterates the smear layer with a strong acid. This creates an opportunity to fill all those tubules that create a potential for problems. Research has shown that utilizing the smear layer in self-etch mode can provide superior dentin bond strength to a total-etch technique in relation to length of time in service.
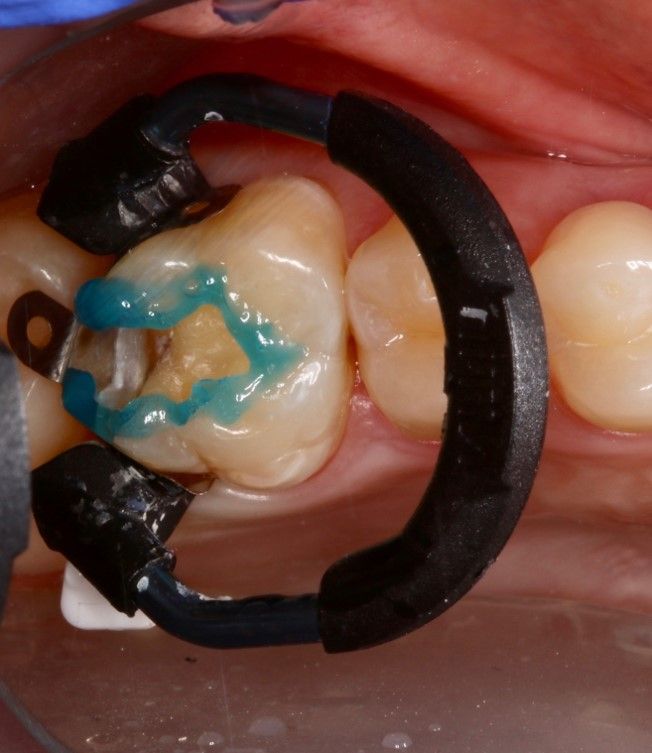
Although I always leave my smear layer intact, I do clean it. I use Clean & Boost® Dentin and Enamel Cleanser from Vista Apex (Figure 11). Nitric acid, combined with disinfectants and HEMA, allows the cleanser to interface through the smear layer and remove any contaminants that may inhibit adhesion. The pH level encourages roughening of enamel and dentin but is less aggressive than phosphoric acid. Clean & Boost also reportedly increases bond strength up to 33% by cleaning but not obliterating the smear layer.
I always use a selective-etch on the enamel margin using Best-Etch™ Phosphoric Acid from Vista Apex (Figure 12). I believe any time dentists can etch enamel, they should take advantage of it. It is still the most tried-and-true bond in dentistry.
Proper Light Curing
Half of all dental income (and clinicians’ success and reputation) relies on the successful use of light-cured dental materials.2,3 The consequences of improper light curing are:
- lower bond strength,
- weaker properties,
- microleakage,
- sensitivity, and
- recurrent decay.
When choosing a curing light, dentists should understand its power output, spectral output, collimation, and surface area footprint.
The power output of the curing light should be a minimum of 1000 mW/cm2 of light energy. At that output for 10 seconds, clinicians should be able to cure most products today. So, how do clinicians know the exact power output? I highly recommend investing in a radiometer. I really like CheckUp 2.7 from Bluelight Analytics because it not only measures the light but also gives specific recommendations based on the materials used. With any radiometer, though, clinicians can check the consistency of the light.
Spectral output is interesting because the materials used today have different types and amounts of photoinitiators. For example, the Ivocerin photoinitiator falls under a different spectrum, requiring a broader spectral output range. Many lights are built for camphorquinone curing only, so clinicians should check the light’s spectral output.
Collimation is a critical factor. Light that isn’t collimated will not give the full benefit of a broad spectrum to the entire restoration. Collimation can be checked by shining a light on a table to see where the energy is going.
Light-curing areas save time and help when it comes to human error. I cure all my own restorations (I’m a control freak), but if dentists are looking away from the light or shifting positions, that is likely moving the head away from the target.
I use the PinkWave™ curing light from Vista Apex for its expanded wavelength, providing broad spectral coverage(Figure 13). The light also has a red and near-infrared diode that has shown to cause a decrease in composite shrinkage and increased polymerization. The PinkWave is also said to have the largest curing area on the market at 12.1 mm, helping to navigate larger restorations.
Adaptation of Material
Whether layering incrementally, 2-step, bulk fill, or any other type of strategy, dentists always have to manipulate their composite. According to results from an American Dental Association Clinical Evaluator Panel report, 70% of dentists are doing some form of incremental layering approach.
When it comes to incremental layering, I find that heated composite improves my results. Research has shown that heated composite has multiple benefits, including increased durability and better wear rates, fewer voids and microleakage, and lower viscosity.
There are several options out there for composite warming. For compules, I like the Phasor™ from Vista Apex, which heats within 20 seconds and keeps a constant heat and flow to continually heat and reheat composite material.
Every clinician should have a wetting resin, which allows for the manipulation of material without causing any residual pull back. I mostly use SeamFree from Vista Apex because it is unfilled (Figure 14). Once cured, an unfilled resin will become incorporated into the composite, leaving clinicians with no lines or stains.
At the end of the day, everyone wants a tightly packed composite that is highly filled and anatomically beautiful, with ideal contact points. Some of the tips and tricks mentioned here will help achieve this goal with fewer headaches.
References
- Overton JD, Sullivan DJ. Early failure of Class II resin composite versus Class II amalgam restorations placed by dental students. J Dent Educ. 2012;76(3):338-340.
- 2005-06 Survey of Dental Services Rendered. American Dental Association; 2007.
- Revenue of dentists (NAICS) in the United States from 2009 to 2014. Statista. April 15, 2014. Accessed February 28, 2021. http://www.statista.com/statistics/296642/revenue-dentists-in-the-us










 Download Issue: Dental Products Report April 2021
Download Issue: Dental Products Report April 2021

