- About Us
- Advertise
- Editorial
- Contact Us
- Terms and Conditions
- Privacy Policy
- Do Not Sell My Personal Information
© 2025 MJH Life Sciences™ and Dental Products Report. All rights reserved.
How COVID-19 will change dentistry
Dental practices tend to focus on the economic realities of the practice. However, post-pandemic, practices might also begin to focus on patient-centered outcomes like consistency of care, interaction with staff, and infection control.
My ex-husband was a lover of trivia, and he longs for the good old days when Trivial Pursuit was THE essential game for any successful party or family gathering. Too bad people can sneakily look up the answers on their smartphones under the table these days. Not fair. Not British (he’s an Englishman).
Anyway, this-along with all the social isolation-made me wonder if most people know the meaning of the word ‘quarantine.’ It’s actually linked to the Lenten season of the Christian church.
The Bible says that Jesus spent forty days in the wilderness to ponder his fate and purge and purify himself.
During the medieval period, when the cause of disease, especially Plague, was not understood, it was noted that a group of people who isolated themselves completely from all contact with the outside world would not become infected. Well, if forty days was good enough for the purification of Jesus, it must surely be good enough for anybody, and therefore that was the recommended isolation period. The old Italian word for ‘forty days’ is quarantena.
This pandemic reminds me of a ‘plague village’ I visited several times in the county of Derbyshire, England called Eyam. The people of this community voluntarily isolated themselves, after they discovered the Plague amongst them in 1666. Three-quarters of the population of that community died, but they did not die in vain. They helped halt the spread of the disease. Their names are remembered today on plaques next to the door of their homes. In some houses, a whole family died alone and unaided.
How will dentistry be remembered during this pandemic? Will we be remembered for slowing the spread of coronavirus by closing our doors and postponing non-essential or non-urgent dental care? Will our quarantena be remembered as a selfless and responsible act? It certainly will be, and I applaud all who made a decision to protect both employees and patients. Dentists, dental hygienists, and other dental professionals are at very high-risk of occupational exposure to COVID-19.
Tech firms are becoming more powerful as a result of this pandemic and patients will continue to be tech savvy on their smart phones.3 Primary healthcare digital technology will become more prominent and many patients may want to communicate with you and your staff online, especially if you have established good relationships with them. Teledentistry provides a method for virtual dental consults safely and easily and we may see a growth of this technology in the U.S. The telemedicine market is booming and the acceleration is due to the COVID-19 pandemic. Teladoc and AmWell telemedicine giants are continuing to add more companies regularly.4
Throughout the COVID-19 pandemic and even afterwards, many minds will be racing to record lessons learned. I recently read a comment from a director of an intensive care unit in Wuhan, China which stated if he could do it all over again, he would have pushed health care authorities harder in hospital intensive care units to better establish best practices for critical care.1
What does that mean and how does it apply to dentistry? In medical and in dental practices, best practice is defined as the “best way” to identify, collect, evaluate, disseminate, and implement information and monitor outcomes of healthcare interventions for patients/population groups and well-defined indications of conditions. For example, hospitals are constantly conducting surveys in order to give patients a positive experience, a sense of satisfaction, and the feeling they come first. Hospitals compete to promote the idea of patient-centered care.
U.S. dental practices tend to focus on the economic realities of the practice, which in turn affects where and how dentists can practice. However, post-pandemic, practices might also begin to focus on patient-centered outcomes like consistency of care, interaction with staff, and (surprise, surprise) infection control.
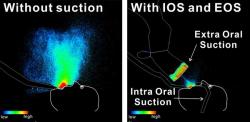
Patients may expect closer attention to infection control measures, which are easy to overlook in a hectic practice environment. Gone will be the “prophy mills’ where dental providers are working in a ‘fast food’ dental environment without adequate time for the provision of safe care. Patients will come to expect appropriate infection control policies and procedures, and I envision a future clinical environment where all clinicians are wearing disposable gowns, face shields, face masks, gloves and any new OSHA PPE recommendations that modify existing guidelines. We have to be very thoughtful and careful before we re-open dental practices and our decisions about infection control must be evidence-based. The role of the infection control coordinator needs to be prioritized because it can strengthen the focus and implementation of safety controls for dental providers and patients.
OSHA guidance on preparing workplaces for COVID-19
OSHA has issued COVID-19 workplace recommendations, which focus on the need for employers to implement engineering, administrative and work practice controls, and personal protective equipment (PPE).3 This includes an infectious disease preparedness and response plan that can help guide protective actions against COVID-19.3 Basic prevention measures include policies and procedures for prompt identification and isolation of sick people, including immediately isolating people who have signs and/or symptoms of COVID-19. Workers who are exposed should be classified and OSHA offers guidance on exposure risk levels based on task.
Very high exposure risk jobs are those individuals who work in jobs with high potential for exposure to known or suspected sources of COVID-19. Dental workers who perform aerosol-generating procedures and exams or invasive specimen collection on known or suspected COVID-19 patients, some dental procedures and exams, or invasive specimen collection on known or suspected COVID-19 patients fall into this category. Read the OSHA booklet and implement control measures described for all workers in low or high-risk categories.3
Evidence-based dentistry
Now is a good time for dental professionals to learn and adopt best dental practice by adopting evidence-based dentistry (EBD). Dental hygienists and dentists are behind medical providers in their understanding and commitment to this discipline and I notice this discrepancy when chatting with nurses and physicians. How many dentists and hygienists have the knowledge and skills which enable them to search for and apply best evidence? For example, if a patient asks you which powered toothbrush has the best outcomes, will you be able to find a reliable source online and look for systematic reviews on the topic? Do you know what a systematic review or meta-analysis is? Are you able to discuss your decision-making with a patient in a way that lets them know that you are familiar with the strength of the evidence to support a given treatment protocol? Can you justify your treatment recommendations based on clinical practice guidelines to control early childhood caries? Do you even know where to look in the literature for evidence based, chronic disease management? Have you ever read an article in the Journal of Evidence Based Dental Practice or spent time reading evidence summaries in the Cochrane Oral Health library? (cochrane.org)
In the past, dental professionals didn’t always have access to the latest dental research. They often made decisions on how to treat patients or make recommendations based on their own judgment, a colleague’s opinion, or what they learned in school. Practicing dentistry and dental hygiene this way is outdated and not reliable for patients and it is not always what research shows is best. Researchers, on the other hand, study large numbers of patients and work hard to be objective in their findings. They know that dental knowledge changes constantly. What we consider factual today is obsolete tomorrow and treatment protocols change based on new and improved research and clinical trials.
Individuals who apply EBD to patient care learn how to look at all of the evidence and they know how to judge it objectively. In learning how to evaluate the literature, a dental professional is practicing EBD. Having a working knowledge of EBD will be essential in a post-pandemic dental environment. Short-term and long-term consequences of COVID-19 are unknown and many patients’ lives may be at stake for a long time to come. Dentists, dental hygienists, dental therapists, and dental assistants may move into the role of more significant team members in the care of patients with chronic and acute healthcare issues and professional collaboration between medical and dental healthcare professionals is expected to increase in the future. A shortage of primary care physicians may lead to a redistribution of tasks in dental clinics/practices to include screening for chronic diseases.
To begin compiling an EBD toolkit, start with the ADA EBD training programs and you can access YouTube videos and written material online: .ada.ebd.org. When communicating with patients, I frequently reference clinical practice guidelines which are designed to optimize patient care and assess benefits and harms of alternative care options. I share these guidelines with my patients. Take a look at ADA’s clinical guidelines here: https://ebd.ada.org/en/evidence/guidelines
Patients are becoming more sophisticated and they will continue to challenge you on multiple levels. As nearly ¼ of the world’s 7.8 billion people are, for the most part, stuck in their homes, daily life remains uncertain. When patients return to their habits, like regular dental checkups, keep in mind that they will need reassurance that dental providers are delivering safe, high-quality care. Today’s providers must be tech savvy and proficient at accessing journal articles and databases like PubMed and Cochrane Oral Health, which specializes in meta-analysis of dental research.
In addition to staying home and binge-watching Netflix and Hulu, take the time to learn EBD. Start at www.ada.ebd.org and become familiar with systematic reviews on various topics. Another source of systematic reviews for evidence-based dental practice is found at: www.dentalelf.org. Eventually, you’ll begin to understand the evidence pyramid and how to evaluate the strengths and weaknesses of a study or online resource. The discipline of informatics (science of how to use data) and evidence-based dentistry and medicine are here to stay. Being held to a higher standard is important for a number of reasons. Professional expectations guide us on proper protocols and give dental providers an objective standard to evaluate each other. High standards also provide consistency throughout the profession so that patients receive quality care.
Patients will return post-pandemic, but they may scrutinize the dental profession more closely, especially safety issues. Putting best evidence into practice is a good start in an uncertain environment.
References:
- https://fortune.com/2020/03/05/lessons-treating-coronavirus-doctors-wuhan-covid-19/
- https://www.aljazeera.com/news/2020/03/world-coronavirus-pandemic-200326055223989.html
- https://www.osha.gov/Publications/OSHA3990.pdf
- https://www.forbes.com/sites/leahrosenbaum/2020/03/26/the-coronavirus-has-created-a-surge-of-telemedicine-demand-goodrx-now-lets-consumers-compare-services/#24d2c94247f5