High-Velocity Hot Air Dental and Microsurgical Instrument Sterilization
High-velocity hot air sterilization systems provide optimal sterilization for dental instruments and eliminate corrosion.
Traditionally, steam sterilization has been the primary mechanism to sterilize dental and medical surgical instruments. However, advances in sterilization have provided another thermal sterilization technology that uses high-velocity hot air to effectively sterilize instruments in significantly shorter time periods without water, thus eliminating instrument drying and instrument corrosion.
With concurrent advances in heat-resistant materials, most dental and microsurgical instruments are compatible with the temperatures employed in the hot air sterilization process. Shorter sterilization processing cycles result in reducing expensive instrument investment and assuring efficient instrument use. Eliminating instrument corrosion provides a longer life span of delicate, costly instruments, lowering dental practice operating costs.
The History of Dry Heat
The resurgence of dry heat as a legitimate sterilization technology began in 1960 with work conducted by NASA for ensuring the sterility of lunar and planetary spacecraft. Conducted at the Army BioLabs at Fort Detrick, Maryland, under the direction of Dr Charles R. Phillips, this work led to the selection of dry heat as the only viable sterilization option for total sterilization of planetary and interplanetary spacecraft. Dry heat sterilization technology was first used on the Mars Viking 1 and 2 landers in the mid-1970s and continues to be used today as the primary method for sterilizing all planetary and interplanetary spacecraft, including the latest Mars lander, Perseverance.
Conventional passive and low-velocity dry heat sterilization has never gained popularity for medical instrument sterilization, primarily being limited by the lengthy sterilization times (1 hour at 340 °F; 1-2 hours at 320 °F) as required of the sterilization process. However, in the 1980s, Keith Cox, DDS, observed that increasing heated airflow to an instrument significantly increased bacterial spore destruction rates.
This observation inspired Dr Cox’sdevelopment of the patented Cox RapidHeat™ Sterilizer from CPAC Equipment, which resulted in a marked reduction in the time required for instrument sterilization, going from hours by conventional dry heat sterilization to minutes at 375 °F in the Cox RapidHeat Transfer Sterilizer. The device was granted 510(K) status from the United States Food and Drug Administration (FDA) in 1987 and 1988 as a Class II (performance standards) device.
Since then, High-Velocity Hot Air (HVHA) sterilization has been recognized and validated for use in health care applications including medical and dental offices, laboratories, ambulatory care clinics, and hospitals by the Centers for Disease Control and Prevention in their publications Guidelines for Infection Control in Dental Health-Care Settings—2003 and Guideline for Disinfection and Sterilization in Healthcare Facilities (2008).1,2 Standards for use and process validation have been issued under the auspices of the American National Standards Institute and the Association for the Advancement of Medical Instrumentation in the standards ANSI/AAMI ST40:2004(R)2010 and ANSI/AAMI ST50:2004(R)2010.3,4
Dry Heat Sterilization Basics
There are 3 distinct types of dry heat sterilizers as distinguished by their degree of air convection, with “convection” being defined as the transfer of heat due to the bulk movement of molecules within fluids. Dry heat sterilizers utilize moving air as fluid to transfer heat from the air to medical instruments. These sterilizers are categorized as: (1) static or passive hot air sterilizers, in which air convection is generated solely by gravity as hot air rises and cooler air descends; (2) mechanical low-velocity forced-convection sterilizers, in which heated air is moved at less than 20 air changes per minute to minimize hot and cold areas within the chamber; and (3) HVHA sterilizers in which air is moved at a high rate, such as 200 air changes per minute, in which high-velocity flowing air amplifies the rate of heat conduction and improves the uniformity of temperature.
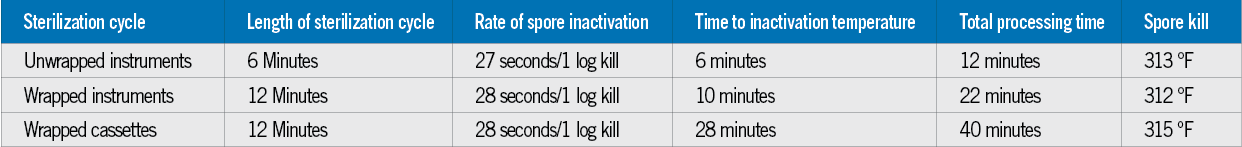
Dry heat functions to sterilize by transferring heat to the microorganism, causing the inability to reproduce due to DNA and enzymatic damage. Time-temperature profiles have been established for wrapped instruments, unwrapped instruments, and handpieces to deliver a sterility level of 6 log10 plus an additional 6 log10 sterility assurance level (SAL) representing a total microbial inactivation level of 12 Log10 of Bacillus atrophaeus sporesas required by FDA and ANSI/AAMI standards. CPAC Equipment’s Pro-Series HVHA™ sterilizers (Figure 1) operate at 375 °F under varying processing times, dependent on whether the instrument is unwrapped (12-minute exposure), wrapped (22-minute exposure), or within wrapped cassettes (40-minute exposure). Times expressed are from the start of the process to its completion. No drying cycle is required (Table).
The total instrument processing time is an additive combination of the time required to raise the instrument’s temperature to initiate spore kill and the time necessary to kill 6 log10 B atrophaeus spores plus the additional 6 log10 spore kill required for the SAL (Figure 2). The instrument preheat time difference between unwrapped (6 minutes) and wrapped (10 minutes) is due to insulation barriers created by the nylon pouch and the associated entrapped air, which causes the time difference of 4 minutes in reaching the spore inactivation temperature on the instrument.
Once spore kill is initiated at the temperature of 313 °F to 315 °F, spores are killed at the same rate of 27 to 28 seconds per 1 log10 kill for unwrapped and wrapped instruments and for wrapped cassettes (Table). The total processing time needed to meet the FDA-required 12-log10 kill is 5.6 minutes plus the required preheat time.
Instrument and Materials Compatibility
As with any thermal sterilization device, temperature compatibility with all intrinsic instrument components is imperative. For an HVHA sterilizer operating at 375 °F, most of today’s instruments and their components are constructed with materials that would not be subjected to damage at this elevated temperature. Standard handpieces, pliers, and cutters are typically composed of 440C stainless steel or other high-temperature–resistant metals (including solders). The temperatures used in dry heat sterilization whether static, low-convection, or HVHA processes do not contribute to corrosion or the stressors that dull, pit, or crack instruments. Surgical stainless steels used in biomedical applications are also used in industrial applications requiring thermal compatibility in excess of 2000 °F due to their ability to provide good strength and good resistance to corrosion and oxidation at these elevated temperatures.5
For instruments that contain plastic or other nonmetal components, there may be susceptibility to repeated exposure of 375 °F, although most nonmetal components compatible with a steam sterilization process are also compatible with exposure to 375 °F. Changes in color, cracking, or other alterations in physical appearance are visible indicators that the elevated temperature is affecting the material and could alter the instrument’s performance.
In recent years, the creation of more heat-tolerant materials (eg, heat-resistant fluoropolymers and silicones) and their replacement of heat-intolerant materials used in medical devices has reduced significantly the number of instruments that are intolerant to the dry heat sterilization conditions. Dental handpieces contain bearing retainers and O-rings made of high-temperature–resistant materials (typically Torlon®, Viton™, phenolics, and polyimides) tolerant to 375 °F temperatures employed in the HVHA sterilizer. Temperature resistance for these materials is over 450 °F. Lubricants must be rated food-grade, withstand a temperature higher than 450 °F (eg, SteriLUBE™ or similar fluorinated synthetic), and not contain any hydrocarbon-based materials such as mineral oil to avoid any temperature incompatibilities. Results from a 2020 study by The Dental Advisor showed that there was no performance decrease in new and used handpieces tested after 250 sterilization cycles in the RH-Pro11 when using the fluorinated high-temperature cleaning and lubricant system, SteriKleen™ and SteriLUBE.6
Significant with any hot air sterilization method is the dry conditions that minimize or eliminate instrument corrosion. With any chemical or steam sterilization method, chemicals and/or water react with metals and corrode. Corrosion affects the ability to properly sterilize an instrument and the instrument’s efficacy of use, resulting in shortening the effective lifetime of an instrument. Instrument exposure to chloride environments (eg, cleaners and disinfectants) is a primary source for pitting and cracking regardless of a wet or dry heat sterilization process. However, a wet heat sterilization process amplifies the corrosion process and significantly affects an instrument’s material integrity. On the other hand, dry heat sterilization is a moisture-free process that does not provide the conditions necessary to promote corrosion. The temperatures used in dry heat sterilization, whether static, low-convection, or HVHA processes also do not have an impact on corrosion or any other stainless steel stressor.
Instrument Turnaround
To minimize expensive instrument inventory and ensure efficient instrument use requires a quick turnaround of instruments from one patient to the next. Often, instrument sterilization is the most time-consuming operation in the preparatory process. All thermal sterilization processes are time and temperature dependent, and sterilization times cannot be cut to expedite the process. Comparison of times required of steam sterilization and HVHA sterilizers must accurately reflect the total time required from when the instrument is placed into the sterilizer until the time it is removed. Complete steam sterilization processing time includes (1) the time necessary to achieve the required temperature and pressure (2) the sterilization cycle time and (3) instrument drying cycle time.
Operational Requirements and Logistics
HVHA sterilizers were developed primarily for use within dental clinical practices, and as such, the sterilizers are small, designed for tabletop use (Figure 1) or to be portable by placement on a moveable cart. HVHA sterilizers typically operate on 110 to 120 V or 220 V. They are energy efficient (ie, 1400 watts for the initial warm-up stage at the beginning of the day and 300 watts during the sterilization cycle). HVHA sterilizers require no water or stream for operation, making their placement contingent only on the availability of conventional or field-generated electricity.
Standard controls minimize error and make the operation of the unit easy for dental or medical staff. Controls are limited to an on/off switch and preprogrammed cycle time designations (eg, wrapped, unwrapped, or handpieces). Operationally, the sterilizer is turned on at the beginning of the day and turned off at the end. The sterilizer typically requires approximately 15 minutes to initially heat to operational temperature. Once the chamber is at operational temperature, the sterilization cycle is automatically initiated. The operator is notified at the completion of the cycle, and the instruments are removed from the unit and allowed to cool before use. (Figure 3 for automated operational screen sequence). All sterilization cycle data are internally stored and retrievable through a flash drive for computer or hardcopy documentation.
Use of the RH-Pro11 and RH-Pro9 for N95 Respirator Decontamination
The use of HVHA technology was investigated for use to decontaminate N95 respirators and masks for reuse during their severe shortage caused by the coronavirus disease 2019 (COVID-19) pandemic. Published peer-reviewed reports have demonstrated that dry heat processing is the preferred method to assure that both viral inactivation and N95 respirator performance efficacies are maintained for numerous reuse cycles.
CPAC Equipment, Inc, has repurposed their RH-Pro11 and RH-Pro9 sterilizers for N95 mask reprocessing by developing a dedicated decontamination cycle based on a documented time-temperature parameter of 176° F for 30 minutes to inactivate severe acute respiratory syndrome coronavirus 2 cells without interfering with mask filtration and breathability performance for up to 20 reuses. RH-Pro11 and RH-Pro9 units can process up to 96 and 24 pouched masks per hour, respectively. Repurposing RH-Pro11 and RH-Pro9 sterilizers for respirator decontamination is performed by a simple flash drive upload of N95 mask decontamination software. A similar process using the appropriate RH-Pro11 or RH-Pro9 software will convert these units back to their original sterilization function. The RH-N95 Decontamination System meets the FDA criteria for emergency use authorization during the ongoing COVID-19 crisis.7
Summary
HVHA sterilization technology is an excellent instrument sterilization option for any dental practice. A moisture-free and water-free environment eliminates instrument corrosion issues that dull and limit the useful life span of the delicate instruments used in dentistry. The short sterilization cycles and the elimination of drying provide a rapid turnaround of instruments, resulting in timely availability for the next patient and minimizing instrument inventories. Preset time-temperature parameters and automatic controllers ensure sterilization for each cycle. These sterilization parameters are recorded and stored within internal memory for retrieval via a USB port for external storage or hard copy printouts, providing the data necessary to document sterilization conditions for each treatment cycle. ●
References
- 1. Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM. Guidelines for infection control in dental health-care settings–2003. Centers for Disease Control and Prevention. December 9, 2003. Accessed June 6, 2013. http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5217a1.htm
- 2. Guideline for disinfection and sterilization in healthcare facilities (2008). May 24, 2019. Accessed June 6, 2013. https://www.cdc.gov/infectioncontrol/guidelines/Disinfection/index.html
- 3. Table-top dry heat (heated air) sterilization and sterility assurance in health care facilities. Advancing Safety in Health Technology. January 12, 2018. https://my.aami.org/aamiresources/previewfiles/ST40_reaff_2018_preview.pdf
- 4. American National Standards Institute and the Association for the Advancement of Medical Instrumentation “Dry heat (heated air) sterilizers,” ANSI/AAMI ST50:2004(R)2010. Accessed October 15, 2014.
- 5. Design guidelines for the selection and use of stainless steel. Nickel Development Institute. https://nickelinstitute.org/media/1667/designguidelinesfortheselectionanduseofstainlesssteels_9014_.pdf
- 6. Cowen M, Powers JM. HVHA RH-Pro11 sterilization effect on handpiece performance. Dental Advisor. January 28, 2020. https://www.dentaladvisor.com/pdf-download/?pdf_url=wp-content/uploads/2020/03/Vol_37-02-Curing-Lights_WHOLE-ISSUE_v3.pdf 7. Enforcement policy for bioburden reduction systems using dry heat to support single-user reuse of certain filtering facepiece respirators during the coronavirus disease 2019 (COVID-19) public health emergency. US Food and Drug Administration. November 25, 2020. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/enforcement-policy-bioburden-reduction-systems-using-dry-heat-support-single-user-reuse-certain



 Download Issue: Dental Products Report April 2021
Download Issue: Dental Products Report April 2021

