Material Trends: Why Additive Removable Workflows Are the Next Frontier
Over the past decade, demand in the dental industry has driven digital design software development and become a mainstream solution. This drive to expand the functionality of design software platforms is fueled by the staggering disappearance of qualified technicians in the United States. At the same time, this design software evolution drove the development of the technologies necessary for the digital manufacturing of dental restorations, with both additive and reductive technologies proving to be effective.
The winner in the battle between additive and reductive processing is still undecided, but a definite move toward the cleaner and more accurate additive technology is starting to emerge. As these technologies evolve into more functional manufacturing platforms, the race to finding materials to support this digital world has become the new battleground.
When judging new product and technology innovations in the dental industry, there are many potential contenders. Determining the most influential material must be done by evaluating both the material properties and, more importantly, how that technology and material combination influences the broader industry.
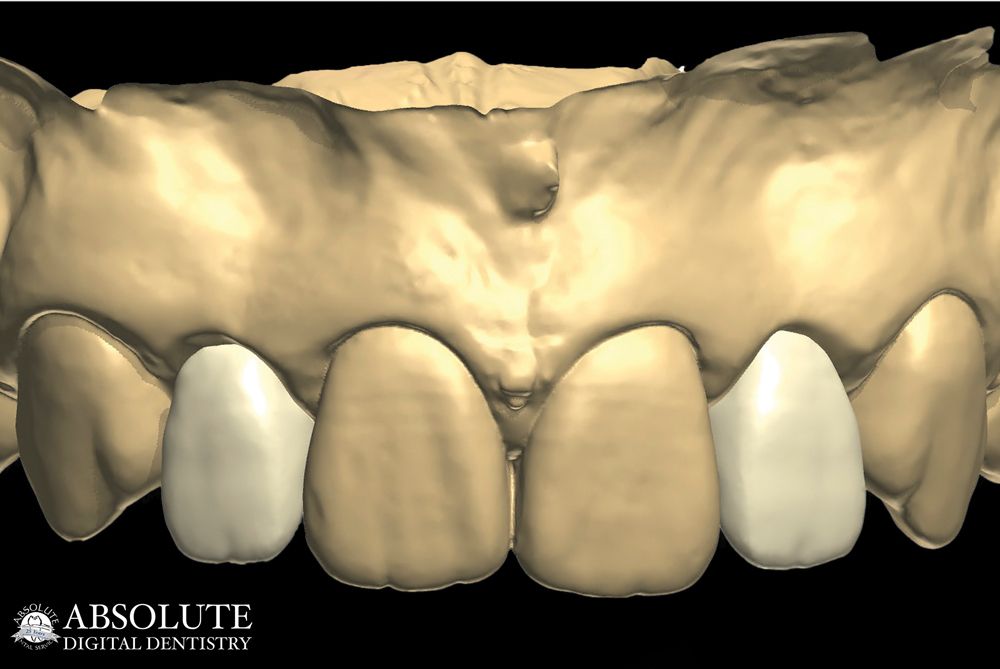
The first material to be considered is undoubtedly high-strength, multilayer zirconia. Over the past few years, great advancements have been made in this industry-changing product. High-strength, multilayer zirconia is now not only a functional material, but also an esthetic material (Figure 1).
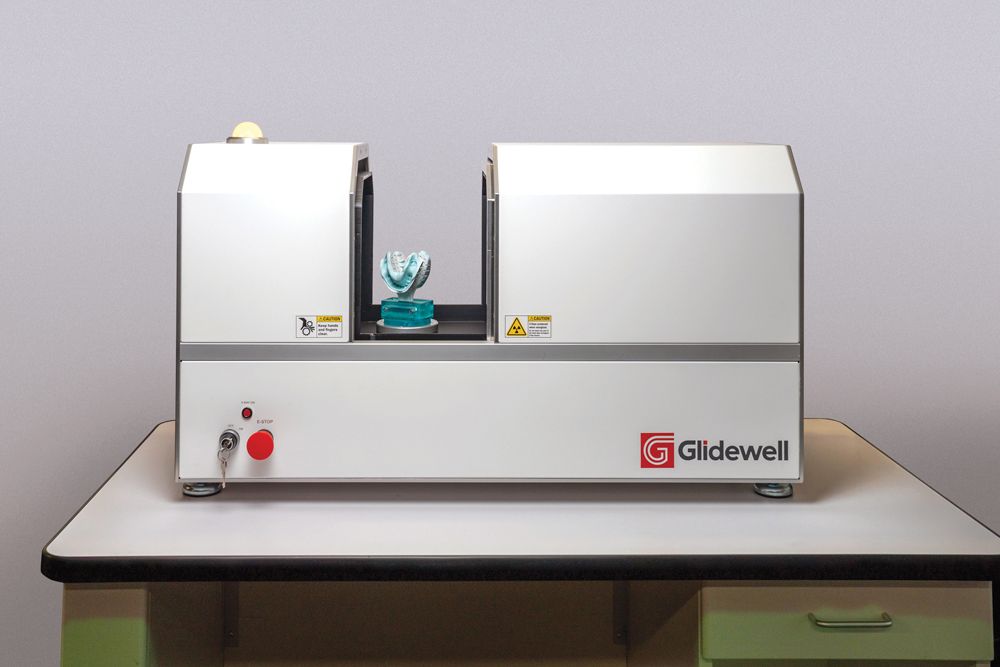
Through this material advancement, the industry finally has a solution capable of eradicating the need for the labor-intensive layered ceramic technique. Furthermore, monolithic zirconia offers a full digital workflow, making it a potential choice for the product of the year (Figure 2).
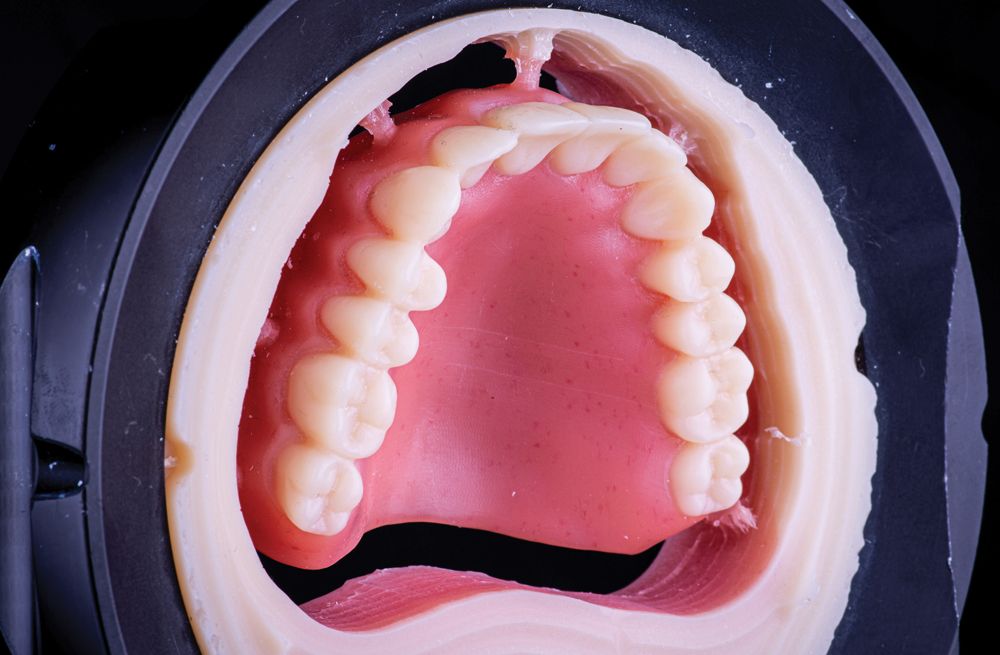
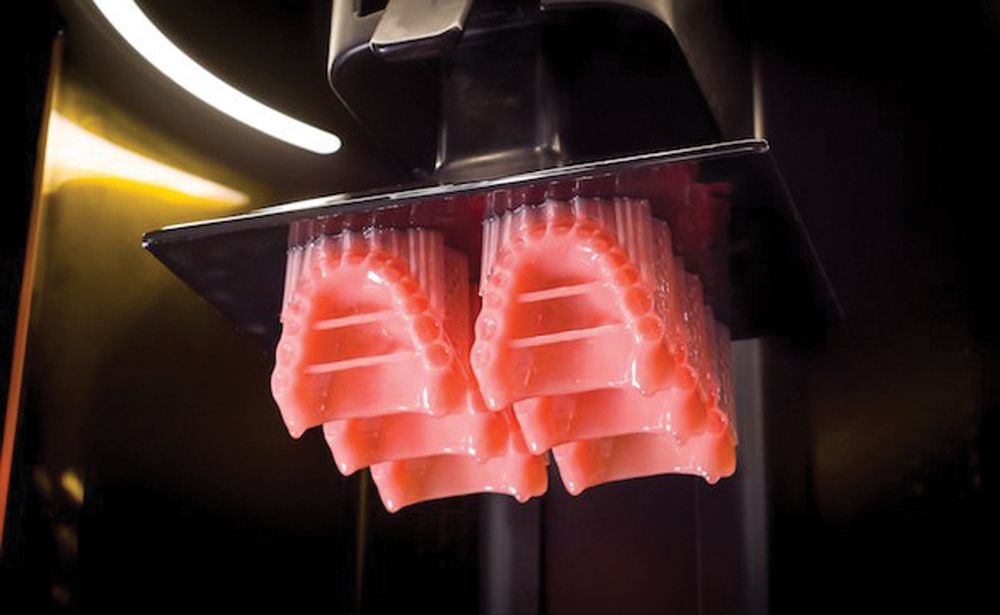
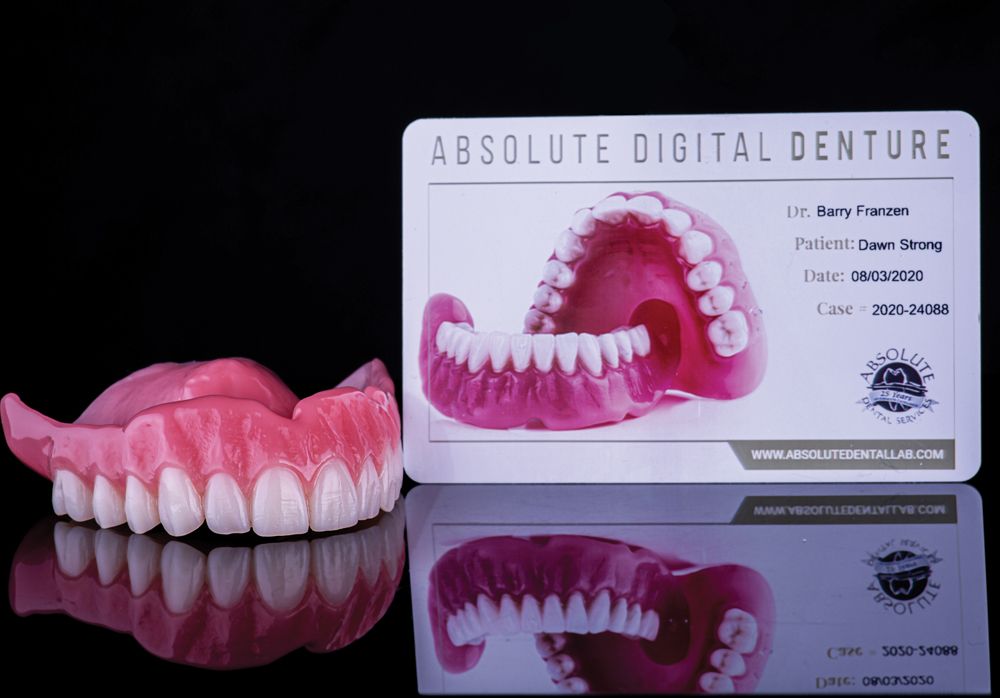
Although there are multiple other materials to consider, printable polymers for denture applications are arguably responsible for finally bringing denture fabrication into the 21st century. Even though reductive technology came to market first (Figure 3), the arduous and expensive nature of this processing technique quickly allowed additive technologies to become a favorite among laboratory owners. First-generation polymers were brittle, translucent, and offered very little strength, but with the launch of products such as Dentsply Sirona’s Lucitone Digital Print (Figure 4) and Desktop Metal’s Flexcera Smile, (Figure 5) an entire new world of predictable, efficient, and economical fabrication is a possibility for the dental laboratory.
The second reason this polymer material, and with it the additive processing technique, should be considered the innovation of the decade, is the way this material has influenced the clinical workflow.
For decades, denture fabrication was seen by dental laboratories as a low-profit product, with the potential of large numbers of postdelivery issues. With clinical issues, such as multiple try-ins and vertical dimension of occlusion discrepancies caused by bite rims, the road to satisfying patients’ esthetic demands and bite concerns was littered with landmines.
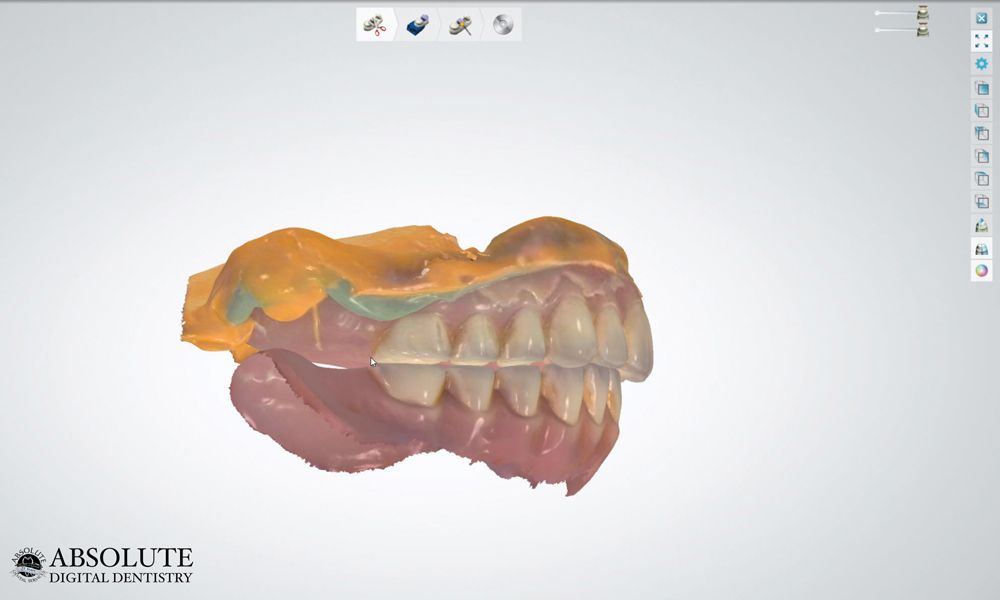
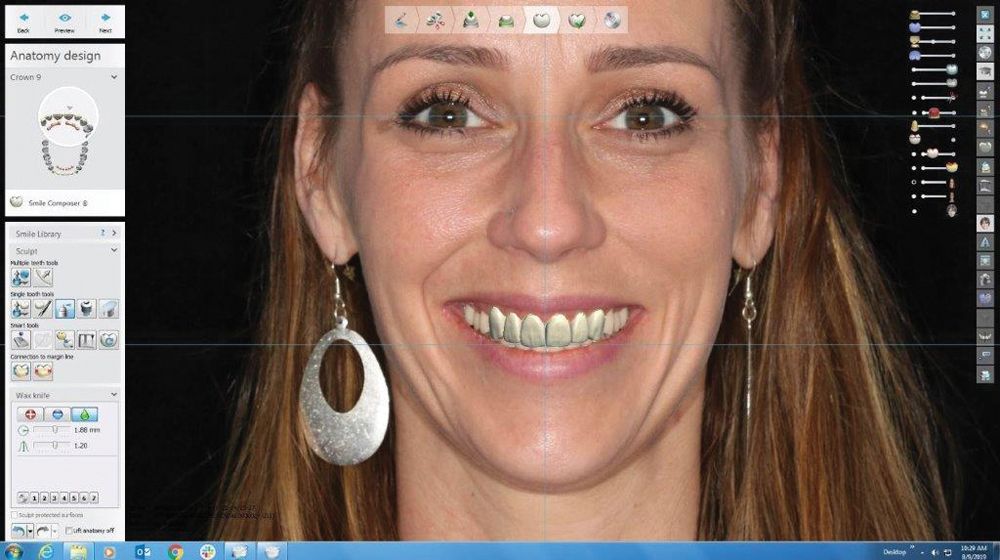
Today, clinical workflows are influenced by digitally driven chairside techniques, allowing the clinician to utilize the existing denture as a prototype starting point for gathering clinical data (Figure 6). In addition to this, smile pictures now allow for remote communication between the technician and the restorative team, and in some cases also involve the patient.
This digital design allows the restorative team to have input regarding the diagnostic design by super-imposing the design data into the patients’ smile pictures. This process is done through accurate STL model matching. This feature also allows patients to experience a digital try-in of the prosthetic device (Figure 7).
Many researchers point to the virtual eradication of postdelivery issues. High spots, bite changes due to processing errors and even base cracks, and teeth debonding have become rare with these new materials.
Design archiving of the patients’ final smiles gives the restorative team the ability to deliver future dentures without requiring additional try-ins. This also provides the option to remake a lost denture from the data without requiring any clinical chair time.
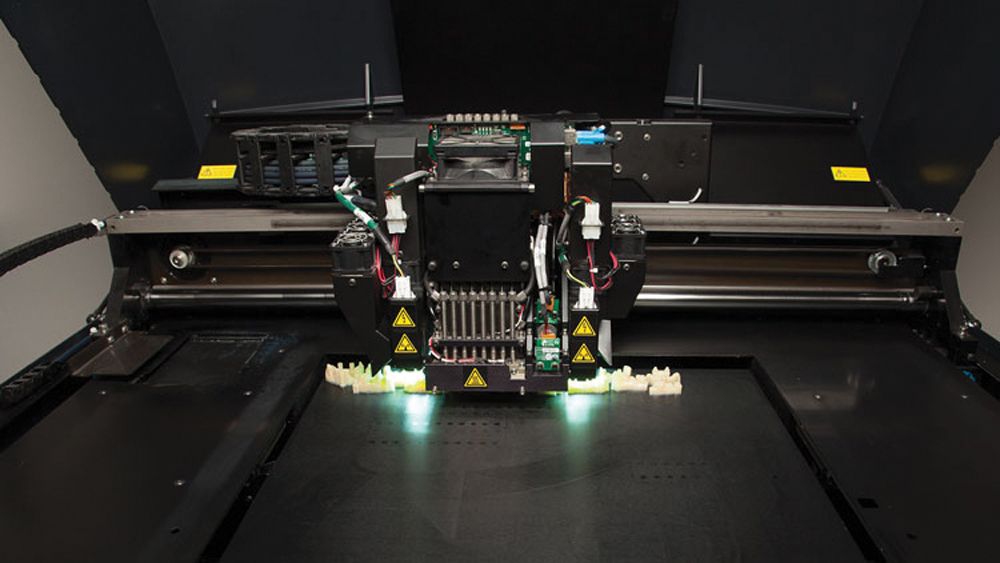
From a fabrication perspective, additive platforms, such as carbon printers, not only allow for scalable (Figure 8) and therefore cost-effective production, but also produce polymers exhibiting fracture resistance almost 3 times that of hand-processed, high-impact acrylics.
In the past, equipment costs were seen as the biggest expenses in prosthetic manufacturing; this was seen as a barrier to modernizing denture production. While traditional techniques require less expensive hardware, the least expensive platform is in many cases no longer the most economical option. The ability to purchase polymer in bulk drives the unit cost down and in some cases, this can even nullify the additional hardware cost of shifting to a digital platform. Consumable costs now have the largest influence on product pricing. It is important to not only consider the equipment cost, but also calculate how the material choice will affect the total unit production cost.
These second-generation polymer materials are ultimately the glue that binds digital design, clinical workflows, diagnostic planning, and communication with production that requires minimal hand processing.
The dental laboratory of the future will most likely continue to struggle with labor shortages, price pressure, and scalability demands. Unfortunately, employing today’s advanced technologies without functional and esthetic materials will not satisfy patient demands.
What was once an equipment and software evolution is now quickly becoming a materials race. Modern-day additive materials will continue to advance at an exponential rate and will undoubtedly continue to influence clinical workflows and processing techniques in a positive way (Figures 9 & 10).
Implementing and mastering the correct combination of these new-world technologies and materials will ultimately define the dental lab of the future.










 Download Issue: Dental Lab Products December 2022
Download Issue: Dental Lab Products December 2022

